Tramadol is a common analgesic that provides its effects by acting as an opioid and serotonin-norepinephrine reuptake inhibitor (SNRI). The opioid portion of its effects mainly comes from a metabolite, O-Desmethlytramadol (O-DSMT), while tramadol itself has a greater impact on monoaminergic systems.
Both the opioid and SNRI effects yield pain relief and mood changes.
It does have recreational effects, perhaps more so in those who are efficient at metabolizing tramadol to O-DSMT, but it’s generally viewed as less intense than an opioid like morphine or diamorphine (heroin).
IUPAC: 2-(7-chloro-1,8-naphthyridin-2-yl)-3-(5-methyl-2-oxohexyl)-3H-isoindol-1-one
A typical dose is 50-100 mg up to four times daily, with administration every 4-6 hours. The max daily dose is 400 mg.
These formulations can be given once or twice per day, with the same maximum dose of 400 mg.
The onset can be fairly slow and peak effects may not arrive until more than two hours have gone by. This varies between users, but the opioid-like effects in particular tend to have a slower onset than the average orally administered drug.
Its duration is dose-dependent, with some people receiving effects for upwards of 12 hours, mostly with strong+ doses.
Though it may not be as intense as typical opioids a lot of people like its longer duration.
It can produce mood enhancing (sometimes euphoric), sedating, and relaxing effects. On average, the physical and mental euphoria is less intense than what can be obtained from a typical pharmaceutical opioid or diamorphine. How intense and pleasurable it is depends on dose and personal factors like genotype. Rarely is it considered an ideal opioid for recreational purposes, so people with access to an alternative opioid will usually prefer it to tramadol, although its tendency to provide a more wakeful and productive state than most opioids is desired by some.
Though it has recreational potential, some people simply do not get pleasurable effects or least not any pleasurable effects that outweigh the negatives enough to justify use. When it lacks mood enhancement and relaxation it may instead just produce restlessness and GI discomfort.
Studies have shown recreational doses of tramadol produce less desirable effects than hydromorphone, but when enough is used (e.g. 350 mg rather than 75-150 mg) it does cause some opioid-type subjective effects (Stoops, 2012 ; Duke, 2011). Tramadol is also associated with more vomiting and less miosis at these doses.
Classic opioid effects like mood enhancement are provided with a slower onset and reduced intensity, including a relative lack of the “rush” provided by some opioids. Users can experience relaxation, giddiness, day dreaming, and they may become somewhat disconnected/dissociated from events. When a user is intentionally relaxing the substance may be more overtly daydreamy and euphoric, whereas those effects can slide into the background when doing something. Waking dream states and nodding are less common with tramadol than with other opioids. Nodding can occur, as can a sense of dissociation or disconnection from your environment and reality, particularly with eyes closed, but those effects are more readily obtained from alternative opioids.
It’s not really stimulating at the physical level, but it is more wakeful than a typical opioid and some users find it reduces the perception of fatigue while working. It can provide relaxation and mood improvement while simultaneously getting people into an attentive, productive mindset. The chance of experiencing productivity enhancement declines as the dose increases. Any potential work enhancement is likely best obtained at low to common doses. For a substantial portion of people it only leads to drowsiness or a desire to do nothing more than low-effort activities. This kind of variability exists with other opioids as well, but the variability in responses could be greater with tramadol.
Tramadol commonly makes people more content doing work they would normally find boring or unfulfilling. Since it provides a more positive valence to nearly everything going on, life is more tolerable and perhaps more enjoyable. Relief of underlying stress, anxiety, or low mood is a typical effect. This quality of the drug, which may be obtained in the absence of significant impairment, is a significant factor in why people become addicted to opioids. Because it can insulate your mind from stressors, a barrier can be constructed between your perception and yourself/the world, which can be positive or negative. It sometimes contributes to emotional blunting, which may interfere with your life. The problematic effects may be a greater issue with chronic use, while the positive aspects of tramadol’s impact on mood could be more substantial with acute use.
Paradoxically, even if someone is in a generally good mood under the influence, they may experience agitation/aggravation and could be more easily irritated than normal. This happens for a minority of users.
Cognitive impairment is not severe at common doses and is usually limited to some brain fog or spaciness. Higher amounts do come with the potential for concentration and memory impairment.
Though it may not always be productive or pro-social, it can make people less anxious and more confident, sometimes contributing to talkativeness.
Sleep can be enhanced or impaired. Some people find it outright makes sleep difficult, though it more often assists with sleep (in the sense of reduced time to sleep onset) but waking up more often through the night is more common. A lot of users report their sleep feels less deep, which is supported by research showing tramadol shifts sleep towards the lighter sleep stages. Although it either doesn’t impact REM or reduces it, dreaming is reported to be more vivid.
Tramadol commonly changes how your body feels, such as inducing sensations of warmth or tingling, along with floatiness (which is more noticeable when moving). Although some people experience jitteriness or an unpleasant heaviness in their body, it seems more common to experience a general sense of comfort. Sometimes the effect is described as similar to being covered in a warm, comfortable blanket. And things you touch may feel softer.
Libido can increase or decrease. Either way, orgasm is harder to reach, which can be frustrating, although this property also underlies its use in premature ejaculation. It can also sometimes reduce the physical pleasure of sexual activity.
Itchiness is usually less significant than with other opioids, but it can occur. When present it is most noticeable around the head and arms/legs.
Constipation, a common problem with opioids, does occur with tramadol acutely and chronically but it’s less significant and less likely to cause severe problems in the long-term. Urinary retention is also often reported, more so by recreational users than medical users.
Nausea and vomiting are common and occur dose-dependently. Sometimes this property forces people to move slowly or remain stationary to minimize discomfort.
Other potential effects include dizziness, appetite reduction, and coordination impairment.
Perception is minimally affected aside from dose-dependent vision blurriness and less often slowness, i.e. things appearing to occur more slowly.
Restlessness and insomnia may occur after the core effects have worn off. Typically it doesn’t have a harsh comedown, but the day after effects can include grogginess, headache/head pressure, dizziness, GI discomfort, and vomiting. Those issues are dose- and time-dependent, occurring more readily with strong+ doses that are taken later in the day.
Historically it was marketed as offering opioid-level analgesia with a lower risk of abuse, addiction, respiratory depression, and constipation. There is some truth to all of those claims, but there is also good evidence showing it can be taken recreationally, physical dependence can build, overdose deaths are possible, and typical opiod-type side effects like constipation do occur in some users. In general the risk of these is reduced, but it is not eliminated, and for some users it can be nearly the same as exists with a drug like oxycodone or hydrocodone.
People should be aware of its opioid nature before they begin taking it. Some of the problems stemming from its use can be tied to patients and doctors operating under the false assumption that it is drastically safer than other opioids and that relatively little caution is needed.
We know that only a portion of its intended and overdose effects come via an opioidergic mechanism. The other main factors are inhibiting serotonin and norepinephrine uptake, which can directly alter pain transmission and provide antidepressant-like effects.
By far the most common use of tramadol is in pain relief. More studies have been conducted on acute pain than on chronic conditions and unfortunately the chronic pain studies tend to be relatively brief, such as a few months, so it’s not always clear if the effects seen in those studies are going to be the same ones seen after years of treatment.
The majority of studies show tramadol is either as effective as drugs like pethidine, NSAIDs, and and oxycodone for postoperative pain relief or it makes up for a moderate reduction in efficacy with superior tolerability. It shows superior analgesia to placebo in effectively all of the research, but there are some studies showing superior outcomes with morphine, aspirin/codeine, and pethidine.
Whether it is the right analgesic in a postoperative setting will depend on tolerability (i.e. nausea and vomiting), patient factors like respiratory concerns, and the kind of operation. While 50-100 mg given orally or via injection is the most common way to use tramadol postoperatively, at least one study found ~260 mg was needed to provide an effective dose for 80% of patients (Thevenin, 2008).
Animal evidence has shown it is effective at reducing pain in models of neuropathic pain and it reduces pain sensation (Kaneko, 2014 ; Miranda, 2011).
Tramadol has shown efficacy in chronic pain conditions including neuropathic pain, cancer-related pain, fibromyalgia, and musculoskeletal pain (MacLean, 2015 ; Finnerup, 2015 ; Schug, 2007). Yet the benefits are sometimes small or inferior to what can be provided by alternative analgesics. The chronic pain studies have usually lasted for only a few months, so it’s unclear if the results are applicable to longer-term use.
There are a couple pharmacological reasons to believe tramadol could alleviate depression. First, it is an SNRI that’s comparable to antidepressants like venlafaxine. Second, opioids are known to have mood-elevating properties, including in the absence of recreational effects.
Little research has been conducted on using tramadol for depression, but there are signs of benefit. One study of people with chronic low back pain and depression found tramadol was significantly more effective than the NSAID celecoxib for alleviating depression, while the treatments were similar for pain and disability scores.
A few case reports have also shown beneficial effects, usually in patients who received tramadol for pain and unexpectedly found it helped with depression. More placebo-controlled research should be carried out to see if the benefits are reliably significant.
Studies in animals found it is antidepressant on its own or when combined with ketamine or SSRIs (Caspani, 2014 ; Yang, 2012). Effects on norepinephrine could be important, since adrenergic antagonists block the beneficial effects of tramadol, while naloxone and serotonergic antagonists do not get rid of the antidepressant properties (Rojas-Corrales, 1998). Other systems, such as imidazoline receptors, could also be involved (Jesse, 2010).
Because it has opioid effects, it has been studied for use in opioid dependence, mostly as a medication to provide during detoxification. It is more effective than clonidine in this setting, similarly effective to methadone, and less effective than buprenorphine (Dunn, 2016 ; Zarghami, 2012). It can alleviate withdrawal symptoms and then be tapered on its own to help patients reach abstinence.
In the US there are still legal barriers to using it for this purpose (Williams, 2016). Scheduled drugs can only be provided for opioid detox if a treatment program is registered with the DEA as a narcotic treatment program and if the FDA has specifically approved the substance for that indication. Tramadol is not approved for opioid dependence, unlike methadone and buprenorphine. There is an exception to this rule, but it only covers three days of treatment (Dunn, 2017).
Tramadol may have local anesthetic effects. It was equally effective to lidocaine when locally injected to provide sensory blockade during tendon repair surgery (Kargi, 2008) and patients given tramadol didn’t need postoperative analgesia, unlike those given lidocaine.
When applied locally it prolongs the sensory blockade offered by mepivacaine (Kapral, 1999). The mechanism of this effect is unknown, but a study in rats found naloxone did not block the local effects of tramadol injection, suggesting it is not coming from an opioidergic effect (Sousa, 2015).
Tramadol has been investigated as a treatment for premature ejaculation (Abdel-Hamid, 2015 ; Kaynar, 2012). Like some antidepressants, it does increase the time to ejaculation, but those benefits could be accompanied by reduced pleasure, anorgasmia, or erectile dysfunction in some people.
Its effect on ejaculation latency could be coming from multiple mechanisms. Opioids are known to inhibit ejaculation, as are serotonergic drugs.
Long-term use of opioids is associated with hormonal changes, including low testosterone, which could potentially inhibit the benefit of long-term daily tramadol use.
It protects against ischemia-reperfusion brain damage in animals and is associated with a reduction in inflammatory processes and oxidative stress (Akkurt, 2018 ; Nagakannan, 2012). Ischemia causes damage in large part from excitotoxicity and oxidative stress. Exactly how tramadol yields these benefits is unknown. One possibility is that opioid receptor agonism activated PI3K/AKT signaling, which has been associated with neuroprotection.
Tramadol can reduce myocardial injury, inflammatory responses, and oxidative stress in animals under ischemic conditions like those caused by myocardial infarction or in some clinical procedures, such as cardiac surgery (Zhang, 2009). However, in patients undergoing coronary artery bypass, tramadol use was associated with worse outcomes as seen by a higher troponin level, indicating greater cardiac damage (Wagner, 2010). The negative finding in the Wagner (2010) paper could be associated with a problematic level of serotonin activity (the dose was fairly high at two administrations of 200 mg and a couple patients showed serotonin toxicity symptoms), which could constrict diseased coronary arteries and exacerbate ischemic damage.
If cardioprotective effects are possible, they may be associated with opioid activity or noradrenergic effects. In rats, KOR and DOR are found on atrial and ventricular tissue, while MOR is absent. Tramadol might have agonist effects at KOR and DOR, providing a potential mechanism of efficacy, since there is evidence that those receptors are therapeutic targets.
Zhang (2009) showed a reduction in NF-κΒ activation. NF-κΒ activation is involved in cardiac ischemia-reperfusion damage.
Similar to the studies on cardioprotection, tramadol reduced ischemia-reperfusion-related damage to muscle tissue and testicular tissue in rats (Asghari, 2016 ; Takhtfooladi, 2014). This was associated with a reduction in oxidative stress.
In humans, tramadol is primarily considered a cause of seizures, especially in overdose. Despite this, it appears to have anticonvulsant properties at low doses in animals, yet those do give way to proconvulsant properties at higher doses.
Though some efficacy may exist for reducing seizures, it’s unlikely to be utilized in humans.
This effect is antagonized by selective KOR antagonists and by naloxone at higher doses (Manocha, 2005)
Tramadol at 1 mg/kg IV and above removed postanesthetic shivering following the administration of general anesthesia, which can lower body temperature (Witte, 1997).
A very small open-label trial showed a benefit effect in treatment-resistant OCD (Shapira, 1997). Some evidence indicates the endogenous opioid system is involved in that condition. Naloxone, for example, makes symptoms worse.
A case series of four people showed it was effective for combat-related PTSD (Geracioti, 2014). It significantly reduced PTSD-specific symptoms like hypervigilance, agitation, intrusive thoughts, and trouble sleeping, while also reducing anxiety and depression.
Neurogenic/neuropathic cough, i.e. cough with no pulmonary, GI, allergic, or otolaryngologic etiology, has been managed by CNS drugs, including gabapentinoids and baclofen. A small study with tramadol found it was also effective at reducing cough severity (Dion, 2017). More research is needed to see if tramadol has significant and reliable antitussive properties.
Tramadol inhibits proliferation, migration, and invasion in breast cancer cells in vitro via a reduction in α2 adrenoreceptor activity (Xia, 2016). The same study showed a beneficial effect in mice with cancer.
Ondansetron reduces nausea and vomiting via 5-HT3R antagonism, a site where tramadol may have direct and indirect effects. 5-HT3 is among the targets implicated in the pain relieving effects of tramadol. A review found combining it with ondansetron led to both a reduction in analgesia from tramadol and a reduction in the antiemetic action of ondansetron (Miotto, 2016).
De Witte (2001) reported significantly more tramadol use in patients exposed to ondansetron, suggestive of reduced efficacy. Patients given ondansetron used 26-35% more tramadol in a postoperative setting.
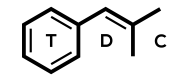
Tramadol has two chiral centers around its cyclohexane ring, giving four stereoisomers: (1R,2R), (1S,2S), (1R,2S), and (1S,2R). Tramadol is sold as a 1:1 racemic mixture of two enantiomeric stereoisomers, namely R,R-(+)-Tramadol and S,S-(-)-Tramadol.
Like codeine, tramadol has a methoxy group that contributes to relatively low MOR binding. In both cases, O-demethylation yields metabolites with stronger MOR agonism, namely morphine from codeine and O-DSMT from tramadol.
Tramadol is cross-reactive with the EMIT II+ PCP immunoassay (Hull, 2006).
Tramadol was reported to be a naturally occurring drug in 2013 when researchers identified it in the roots of Nauclea latifolia, a medicinal plant in Cameroon that is used for pain, malaria, epilepsy, and other conditions (Boumendjel, 2013). Earlier phytochemical analysis had identified alkaloids like the naucleamides, but not tramadol. In this study, a crude extract of the root bark showed potent analgesic activity and was then shown to contain tramadol.
Subsequent studies revealed tramadol is actually a contaminant in the natural environment, not biosynthetically produced (Kusari, 2014). Other research teams were able to confirm its presence in N. latifolia as well as some other plants, but it was exclusively identified in far northern regions and at much lower concentrations than in the Boumendjel (2013) study. When analyzing samples from southern Cameroon, none had detectable amounts of tramadol.
Interviews with farmers in the north revealed it is common to give tramadol to cattle so that they don’t get tired as quickly and it is common for the farmers to take the drug (Kusari, 2014). Tramadol is also given to horses before races. In the southern region this practice is unheard of. The researchers learned that tramadol is available at a very low cost in northern Cameroon, with 12 pills selling for under €1. Further analysis of soil in the the far north revealed the presence of tramadol along with three mammalian metabolites (O-DSMT, N-desmethyltramadol, and 4-hydroxycyclohexyltramadol), all pointing to contamination from mammals in the region.
Lastly, a 2016 study looked at the percent of modern carbon isotope in the tramadol collected from soil in Cameroon (Kusari, 2016). That analysis showed a carbon isotope profile fitting with a synthetic, not natural source. The researchers also found it was impossible to collect enough tramadol in the February 2015 dry season, which followed heavy rains in November 2014. It’s likely that the heavy rains led to leaching of tramadol, a highly water-soluble substance.
Tramadol is mostly considered an opioid agonist and an SNRI, but it does have other effects, such as moderate anticholinergic activity and 5-HT2C antagonism. Inhibiting the norepinephrine transporter (NET) and serotonin transporter (SERT) allows it to alter mood, like other SNRIs, as well as pain neurotransmission through the spinal cord.
The enantiomers of tramadol and O-DSMT provide different effects that function together to cause analgesia. R,R-tramadol has the great SERT inhibiting effect, S,S-tramadol has the greatest NET inhibiting effect, and R,R-O-DSMT is the most potent MOR agonist. All three mechanisms alter pain sensation and a person’s psychological/cognitive state. Because of this, at least in the area of pain relief, the racemate of tramadol could be superior to using a single enantiomer of tramadol or O-DSMT, especially in extensive CYP2D6 metabolizers who are able to receive an adequate level of opioid activity.
(Wentland, 2009) – CHO cells expressing human opioid receptors.
Tramadol is only a weak MOR agonist. Though some binding likely exists during therapeutic use, the substantially higher potency of O-DSMT makes it the primary MOR agonist in humans. Gillen (2000) found R,R-O-DSMT had the highest MOR affinity (Ki=3.4 nM), followed by N,O-desmethyltramadol (Ki=100 nM), S,S-O-DSMT (Ki=240 nM), and racemic tramadol (Ki=2,400 nM).
Chronic exposure downregulates prodynorphin mRNA expression and biosynthesis much less than morphine (Candeletti, 2006). Although Candeletti (2006) did report tolerance in rats when they were given the drug for seven days, so some neuroadaptations did occur, likely in the opioid or monoamine systems.
Unlike morphine, tramadol significantly affects SERT. Barann (2014) reported an IC50 value of 0.93 μM in HEK93 cells. Since micromolar concentrations of tramadol are reached during therapeutic use, this effect is relevant. Low nanomolar affinity exists with O-DSMT (the more potent isomer is R,R-O-DSMT), whereas low micromolar affinity is seen with tramadol (Volpe, 2011 ; Grond, 2004). Significant SERT occupancy is seen in humans, according to Ogawa (2014). Ogawa calculated an ED50 of 98 mg oral (plasma concentration=0.33 μg/mL) for SERT occupancy in the thalamus.
Monoaminergic mechanism seem to contribute to analgesia from tramadol. In healthy volunteers given 100 mg, tramadol increased subjective pain threshold, which was significantly reversed by the α2 adrenoreceptor antagonist yohimbine (Desmeules, 1996). The addition of naloxone to yohimibine effectively abolished tramadol’s effect.
The reported antidepressant properties of tramadol seem to have a serotonergic component. 20 mg/kg IP in rats reversed the physical and behavioral changes cause by chronic mild stress, an effect that was significantly attenuated by a serotonergic lesion (Yalcin, 2008). The tricyclic antidepressant desipramine also lost much of its efficacy in lesioned mice. Yalcin also showed a significant rise in serotonin in the frontal cortex, hippocampus, and raphe nucleus of stressed mice, while not significantly increasing serotonin level in non-stressed mice, indicating it specifically counteracts a stress-induced decline in serotonin.
Some studies have found evidence of increased serotonin release with tramadol (Bamigbade, 1997). This effect was seen with racemic tramadol and its R,R-enantiomer at 5 μM, while S,S-tramadol was ineffective. It appeared to enhance serotonin efflux in a manner that preceded its impact on serotonin reuptake, so although reuptake inhibition occurs at a lower concentration, release could occur at higher concentrations that are still relevant.
Reimann (1998) reported tramadol, like fenflurameine and reserpine, enhanced the basal release of serotonin in rat frontal cortex tissue at 10-100 μM. A selective SERT inhibitor significantly inhibited tramadol’s effect, while abolishing the impact of fenfluramine (Reimann, 1998).
Tramadol 1-10 μM can enhance stimulation-evoked norepinephrine overflow, while not affecting dopamine (Driessen, 1993). O-DSMT has a much weaker facilitatory effect on stimulation-evoked norepinephrine overflow, only increasing it by 17% at 10 μM. Tramadol’s effect was blocked by cocaine (which binds to monoamine transporters), while being unaltered by yohimbine. The effect of tramadol in this study could be coming from reuptake inhibition or from release.
There is some evidence for a role of adenosine receptors, either directly or indirectly, in the effects of tramadol.
Antagonism at 5-HT1A, but not 5-HT1B, significantly enhanced antinociception from tramadol in mice while reducing its antidepressant effect (Berrocoso, 2006). 5-HT1A auto- and heteroreceptors exist in the brain and could differentially be involved in the various properties of tramadol.
Tramadol reduced 5-HT2A-related activity, an effect also seen with morphine (Sun, 2003). This was attenuated by nonselective opioid antagonists and by MOR or KOR selective antagonists, but not DOR selective antagonists.
At a concentration of 10 μM in vitro, tramadol inhibits 5-HT2C in Xenopus oocytes and competitively inhibits serotonin’s binding to the site (Ogata, 2004).
A variety of serotonergic targets, 5-HT7 included, have been implicated in the analgesic effect of tramadol. 5-HT7 receptors are localized in the superficial layers of the dorsal horn of the spinal cord. They are also found in the dorsolateral funiculus, an important source of descending inhibitory signals on spinal pain transmission. In mice with serotonergic lesions caused by intrathecal 5,7-DHT administration, the antinociception from tramadol and O-DSMT was greatly reduced (Yanarates, 2010). Intrathecal administration of a 5-HT7 antagonist also inhibited tramadol/O-DSMT effect, whereas ketanserin and ondansetron did not, suggesting a lack of involvement of spinal 5-HT2 and 5-HT3 receptors (Yanarates, 2010). More research is needed, but the authors hypothesized 5-HT7 receptors localized on spinal inhibitory GABAergic or enkephalinergic interneurons are responsible.
Other studies using different pain models didn’t show an impact of spinal 5-HT7 sites in tramadol’s activity (Sawynok, 2013).
Adenosine receptors are potentially connected to tramadol’s analgesic effect, either directly or indirectly. Sawynok (2013) reported systemic caffeine (an A1 and A2a adenosine antagonist) inhibited tramadol’s antinociception in mice during the formalin test. Inhibition was also seen with a selective adenosine A1 receptor antagonist (DPCPX), but not with a selective A2a antagonist (SCH58261). DPCPX given spinally was effective for inhibiting systemically administrated tramadol, whereas spinally administered SB269970 (a selective 5-HT7) antagonist failed to alter its effect.
How adenosine is involved is unclear. Research has suggested its effect could be secondary to 5-HT7 agonism, which increases cAMP production and subsequently increases adenosine. Yet this study showed no effect of a 5-HT7 antagonist. Other studies have shown an impact of 5-HT7 antagonists on the effect of tramadol in other nociception tests, which could mean the results are test-specific.
Tramadol reportedly inhibits mACh receptors (Shiga, 2002).
State-dependent memory effects caused by tramadol in mice involve muscarinic acetylcholine receptors, although the importance of those receptors (which are known to generally be involved in memory) could be indirect. Physostigmine (an acetylcholine agonist) preadministration reversed the negative effect of tramadol on memory and enhanced the state-dependent memory effect, while atropine (an acetylcholine antagonist) inhibited tramadol’s state-dependent memory effect (Jafari-Sabet, 2016).
The imidazoline I2 receptor is an analgesic target. Agonists like agmatine, which may be an endogenous ligand for I2, have potential antinociceptive properties in animals and agonists at that site can also boost the effect of opioids. Like with other opioids, I2 agonists complement the antinociception offered by tramadol, though that is not evidence of a direct effect of tramadol on I2.
Inhibiting nitric oxide might increase the analgesia from tramadol. Mice given an inhibitor of nitric oxide synthase showed greater analgesia (Dal, 2006).
Nitric oxide may also play a role in dependence. NMDAR activation has been implicated in opioid dependence, with many of the relevant NMDAR-associated actions tied to the subsequent activation of nitric oxide synthesis. A study using N. sativa, a natural nitric oxide inhibitor, attenuated tolerance and withdrawal from chronic administration of tramadol in mice (Abdel-Zaher, 2011). This effect was enhanced by giving an NMDAR antagonist (MK-801) or a nitric oxide synthase inhibitor (L-NAME) with N. sativa.
Tramadol does not significantly affect glycine receptors, it weakly antagonizes NMDARs, and it weakly inhibits GABA receptors (Hara, 2005). Very large overdoses could perhaps reach a concentration where GABAR inhibition is relevant, such as for contributing to seizures.
Tramadol and O-DSMT both suppress activity through the TRPA1 target, though they do not impact TRPV1 activity. Tramadol is more potent at TRPA1 as an antagonist. They were found to reduce allyl isothiocyanate (AITC)-induced Ca2+ currents in vitro in cells expressing the human TRPA1 site (Miyano, 2015).
TRPA1 is an ion channel that is involved in pain (including allodynia/hyperalgesia) and noxious stimuli sensation. It could be important in the analgesia/antinociception provided by tramadol. It is active at that target at low millimolar concentrations, which are reached in humans.
Tramadol reduced menthol-evoked cold pain in healthy humans (Altis, 2009). Menthol is a TRPA1 agonist, so antinociception in that test might be mediated by tramadol’s antagonism of TRPA1.
Tramadol increases activity in the nucleus accumbens (NAc) associated with reward anticipation (Asari, 2018). How this correlates with abuse potential and impulse-associated risks is unclear since the effects of recreational drugs on NAc activity in an anticipant monetary reward task are variable. Tramadol could be altering dopamine activity in reward-related circuits via opioidergic, serotonergic, and/or noradrenergic effects.
Nighttime doses of tramadol increase Stage 2 duration and decrease SWS at 50 and 100 mg. 50 mg did not alter REM, but 100 mg reduced REM duration (Barber, 2011). Since at least part of this change may be coming from a serotonergic mechanism, tramadol’s impact on sleep could normalize with prolonged use, as has been seen with SSRIs.
Polymorphisms in the MOR gene (OPRM1) were shown to predict the response to tramadol in neuropathic pain patients (Liu, 2012). Patients with the A118G variant, which is linked to a reduced response to classic opioids, showed significantly less response to tramadol. Presence of the G allele correlated with a reduction in pain score from 3.1 to 2.6, compared to a reduction from 3.0 to 0.9 in AA patients.
The primary metabolite of interest is O-desmethyltramadol (O-DSMT; M1), which is active and is far more potent as a MOR agonist than tramadol. Other metabolites include N-desmethyltramadol, N,N-desmethyltramadol, N,N,O-desmethyltramadol, and N,O-desmethyltramadol (M5). N,O-desmethyltramadol is also active, while N-desmethyltramadol is inactive.
CYP2D6 catalyzes O-DSMT formation, while CYP2B6 and CYP3A4 are involved in the formation of N-desmethyltramadol. Phase 2 metabolites include glucuronides and sulfates. Under normal conditions in CYP2D6 extensive metabolizers, ~80% of tramadol will initially be metabolized by CYP2D6 (Miotto, 2016).
Metabolism is stereoselective and the kinetic profiles of the metabolites differ. For example, O-demethylation to O-DSMT is 2x greater for S,S-O-DSMT compared to R,R-O-DSMT in vitro (Grond, 2004).
Tramadol is transported across the BBB in a concentration-dependent manner and its transport may involve organic cation transporters (specifically the proton-coupled organic cation transporter, or H+/OC antiporter), which are known to be involved in the uptake of oxycodone, diphenhydramine, and nicotine, among others. Kitamura (2014) reported uptake was significantly inhibited by morphine and other cationic substance in vitro. The unbound concentration of tramadol is greater in brain interstitial fluid compared to plasma, yielding a 1.5 to 2.0 μM concentration from a single 100 mg dose (Kitamura, 2014).
P-glycoprotein is not involved in the brain uptake of tramadol in rats, despite it having some characteristics of a potential P-glycoprotein substrate (Sheikholeslami, 2012).
Bioavailability: ~70%, increasing to over 90% with multiple dosing. Oral absorption is close to 100%, but bioavailability is reduced by first-pass metabolism. Saturation of first-pass metabolism allows bioavailability to increase with multiple dosing, as seen with a 16% higher Cmax and 36% higher AUC value after dosing 100 mg four times per day compared to a single 100 mg dose (Grond, 2004).
Plasma concentration and AUC increase linearly from 50 to 400 mg (Grond, 2004). A 17% higher Cmax and 10% higher AUC is obtained by administering the drug alongside a high-fat meal, but this difference is not clinically significant.
Absorption begins in a few minutes and the absolute bioavailability appears somewhat higher at ~77% (Grond, 2004).
Sustained-release formulations yield a slower Tmax of 4.9 hours. Besides having a longer duration of action, these formulations are useful because they reduce the peak-trough fluctuation in steady state plasma concentration from 121% to 66% (Grond, 2004).
Cmax (after 100 mg of tramadol): ~25% of the tramadol concentration, which would be around 0.075 μg/mL. This will vary significantly based on CYP2D6 phenotype.
AUC: ~25% that of the parent drug (Grond, 2004). This will vary significantly based on CYP2D6 phenotype.
Because CYP2D6 catalyzes its metabolism to O-DSMT, the highly polymorphic nature of 2D6 contributes to different pharmacokinetic profiles in different users and it’s possible that those with very low O-DSMT formation could receive notably less analgesia and efficacy in general. Ultrarapid metabolizers could receive enhanced efficacy and more opioid-like adverse effects.
The bioavailability of O-DSMT was just 3% of the administered dose of tramadol in PMs, while it was 63% in EMs and 86% in UMs (Miotto, 2016). UMs show greater pain relief, greater miosis, and a higher frequency of nausea.
Though some studies don’t show a correlation between CYP2D6 status and analgesic response (Nasare, 2016), multiple studies have shown a reduction in analgesia and opioid-like effects in people with reduced CYP2D6 activity. Kirchheiner (2008) showed that a significant difference in pharmacokinetics between poor and extensive metabolizers, along with a higher pain threshold and pain tolerance induced by tramadol in healthy people. In a patient population, IV tramadol had a much greater non-response rate in poor metabolizers (Stamer, 2007). Various other studies have shown naturally occurring CYP2D6 PM status or PM status caused by a CYP2D6 inhibitor (e.g. paroxetine) leads to a significant shift in pharmacokinetics and a different effect profile (Gan, 2007 ; Laugesen, 2005 ; Poulsen, 1996).
It’s possible that brain CYP2D6 status is also important, such that peripherally acting inhibitors like quinidine may not impact tramadol’s effect profile as much as centrally active inhibitors like SSRIs.
The poor metabolizer (PM) phenotype is found in 6-10% of Caucasians, under 2% of African Americans, and in 1-2% of Asians. PM is the phenotype with the lowest level of CYP2D6 activity, as it stems from two functionally inactive alleles.
The ultrarapid metabolizer (UM) is most common in people from the Middle East and Northeast Africa. According to Ingelman-Sundberg (1999), the UM phenotype demographics are as follows:
Intermediate metabolism (one functionally active and one inactive allele) is most common in Asians. Xu (2014) reports over 50% of the Chinese population has at least an intermediate-level reduction in CYP2D6 activity. The prevalence is similarly high in other Asian countries.
Common CYP2D6 inhibitors include SSRIs (e.g. fluoxetine, paroxetine, sertraline), methadone, and quinidine.
OCT1 mediates the uptake of O-DSMT into the liver, where the transporter is expressed in the sinusoidal membrane of hepatocytes, and therefore OCT1 polymorphisms can affect metabolism. Among Europeans, ~9% have a “poor transporter” profile, which is correlated with a higher plasma level of the cationic drugs taken up by OCT1.
The metabolic path for O-DSMT involves inactivation by glucuronidation in the liver, probably by UGT2B7, which is why the level of hepatic uptake changes the effects of the drug.
OCT1 phenotype was shown to correlate significantly with nausea/vomiting (higher in poor transporters) and exposure to O-DSMT was significantly higher in poor transporters (Stamer, 2016). Greater miosis was also seen in poor transporters in another study (Tzvetkov, 2011).
Clearance is reduced and the half-lives of tramadol and O-DSMT double with renal impairment (Miotto, 2016).
Synthesized by Grunenthal in Germany.
Tramadol became available for analgesia in West Germany. It was sold by Grunenthal as “Tramal.”
A drug monitoring system in Germany reported several instances of tramadol abuse, with half involving known street drug addicts (Dayer, 1994). Because there were relatively few reports of abuse during that time period, it was taken as evidence in support of tramadol’s “low” abuse potential, especially among those without a history of recreational drug use or addiction.
The World Health Organization (WHO) did not recommend a critical review of tramadol in 1992 due to its perceived low abuse liability.
Tramadol launched in Spain in 1992. Between then and 1998, its consumption in the region increased from 2.1 to 570.6 defined daily doses (DDDs) per 1 million people per day. It was one of the only opioids, along with dihydrocodeine and dextropropoxyphene, that didn’t require a special prescription form and that likely contributed to the high usage figures.
It launched in the UK in 1994.
The FDA approved the drug in the mid-1990s and it entered the market in 1995 as an unscheduled opioid. Ortho-McNeil, the American manufacturer of tramadol, ran a postmarketing surveillance program to satisfy a request from the FDA that it carefully monitor tramadol’s use to see if greater restrictions were warranted.
In 1996, Ortho-McNeil released a letter to healthcare professionals advising that “83 domestic reports of an adverse event described as seizures or convulsions” had been reported and that the risk appeared to be higher with SSRIs or TCAs concurrently administered.
Ortho-McNeil’s postmarketing surveillance program found a low abuse rate from 1995 to 1998, with a peak rate of 2 cases per 100,000 exposed patients ~18 months after launch (Cicero, 1999). That rate then declined to 1 case per 100,000 exposed patients. 97% of abuse cases involved someone with a history of drug abuse. The Independent Steering Committee in charge of the program reported in Q1 1996 that it learned from two informants of 6 to 8 impaired physicians who had enrolled in substance abuse treatment due to tramadol use. All of them reportedly described tramadol as a very poor substitute for their drug of choice and they reported using it due to it not being checked for in drug tests and because of its availability.
When the FDA reexamined tramadol’s scheduling in 1998, it didn’t pursue additional restrictions but it did request that the postmarketing surveillance program increase its scope to include data on diversion.
When the WHO noted a significant number of withdrawal and dependence cases in 2000, it recommend a critical review. But in 2002 it decided the available information was not sufficient to recommend international control of tramadol, though it was adequate for the WHO to keep tramadol under surveillance.
Ortho-McNeil’s Independent Steering Committee did not find an increase in the abuse of tramadol from 1999 to 2004, despite new branded and generic products entering the market (Cicero, 2005). As in earlier evaluations of its abuse potential, the vast majority of reported abuse cases involved people with a history of drug abuse.
The postmarketing surveillance program’s data on diversion showed tramadol was only a minor cause of diversion relative to other opioids (Inciardi, 2006). 102 drug diversion investigators from police agencies around the US were contacted beginning in 2002. Those agencies reported 16,755 drug diversion investigations in 2002. Of those, the majority involved more than one drug and hydrocodone was mentioned in 40.1%, benzodiazepines were mentioned in 27.9%, and oxycodone was mentioned in 20.2%. By comparison, tramadol was only mentioned in 1.5%.
In 2002, Iran’s Drug Selection Committee approved tramadol as an analgesic. It was not long after its entrance on the Iranian market that abuse was reported, often among young people.
Global consumption of tramadol increased 42% between 2006 and 2012, according to IMS’ Kilochem data (Abdel-Hamid, 2016). Much of the use has been driven by availability, cost, and allegedly lower risks.
The UK’s Department of Health says prescriptions for the substance nearly doubled between 2006 and 2012 and the National Programme on Substance Abuse Deaths reports there were 2 deaths related to tramadol in 1998, rising to 154 in 2011. Tramadol prescriptions increased 50% in the UK between 2009 and 2011, coinciding with a 77% increase in tramadol-related fatalities (Verri, 2015).
Data from the UK NHS Business Services Authority shows annual tramadol utilization increased from 5.9 to 11.1 million defined daily doses from 2005 to 2012 (Chen, 2017).
Dr. Mahoud Khozendar:
Dr. Taysir Diab, psychiatrist at Gaza Community Mental Health Programme:
Professor Mazen al-Sakka, a pharmacologist at al-Azhar university, believes the problem with tramadol increased following Israel’s blockading of Gaza in 2007.
A UN survey after the December 2008 Israeli offensive found increases in risky behavior and drug addiction, including tramadol addiction (Progler, 2010). Tramadol is relatively easy to get through the black market or from fake prescriptions. An escalation in the use of tramadol was highlighted by Al-Jazeera in its 2010 program “Uncomfortably Numb” which described how illicit pharmaceuticals like tramadol enter the country via Gaza’s large underground tunnel network.
Jamil Al Dahshan of the Anti-Drug Task Force in Gaza said there were 1,204 drug cases in 2009, 591 of which were tramadol-related (Progler, 2010). 2.5 million pills were seized, up from 550,000 in 2008. Some of the tramadol shown in the program had the name “Tramajack,” which is an Indian brand, suggesting international sources for the drug.
A survey of young people in Egypt in 2012 revealed tramadol is a drug of choice (Loffredo, 2015). Tramadol was the most common pharmaceutical drug used recreationally by the group. Its street name is “farawla,” meaning strawberry (referring to the pill’s red color). Around this time, the Ministry of Health released a report on drug addiction in Cairo that estimated 1.4 million people were addicted to drugs, mainly heroin and/or tramadol.
Bassiony (2015) studied its use by adolescents at six schools in 2013. Responses from 204 people were collected, 8.8% of whom tested positive for tramadol. Among those using tramadol, 88.3% used it by itself. Two-thirds of students started with tramadol as their first drug after tobacco. Positive effects included feelings of happiness, having a sense that everything will work out, tension reduction, and relaxation. Negative qualities included lack of concentration, passivity, health problems, anxiety, suicidal thoughts, and becoming inconsiderate.
The UAE cracked down on tramadol use around 2010 in response to an “escalating tramadol phenomenon,” according to a report in Gulf News.
Chief Prosecutor Waleed Ali Khalifa Al Fuqaie, head of Drugs Prosecution at Dubai Public Prosecution:
A study using data from the Clinical Practice Research Datalink, the largest verified primary care database of anonymized clinical records in the UK, reported an increase in the monthly prevalence of tramadol users from 23/100,000 people to 93/100,000 from 2000 to 2014 (Chen, 2017). Most prescriptions were to existing users. The proportion of prescriptions going to existing users increased from 69.2% in 2000 to 91.4% in 2015.
Tramadol became a Schedule 3 controlled drug under the Misuse of Drugs Act in the UK in June 2014. Annual utilization of tramadol declined, as did the number of per capita tramadol-related deaths (Chen, 2017).
Tramadol was mentioned in 12% of drug misuse deaths in England and Wales in 2013, making it the third most common opioid behind heroin/morphine in 41% and methadone in 19%. Of the 254 tramadol-related deaths in that region in 2013, tramadol was the only substance mentioned in 100 (39%).
The Global Drug Survey for 2012 received reports of tramadol use from 369 people in the UK (Winstock, 2013). 90 reported using it to get high, 60 of whom said it came from friends or a dealer, while 18 obtained it through a prescription. 28% reported mixing it with alcohol and/or other drugs to enhance its effects.
Prior to its scheduling tramadol had been fairly easy to obtain from online sources, fueling its nonmedical use for around a decade.
In 2013, the number of prescriptions per year in the US was estimated to be over 44 million (Patterson, 2017).
The US placed it in Schedule 4 in 2014. The DEA received 26 comments on its proposal to schedule the drug: 16 were supportive, 9 were oppositional, and 2 didn’t take a position. Some of the supportive comments mentioned tramadol would remain widely available and that state-level restrictions had been effective at curbing abuse. The oppositional comments focused on concerns about restricted access, which could push legitimate patients to the black market. The DEA argued Schedule 4 drugs are easily accessible for legitimate medical use. Schedule 4 was picked based on tramadol having a lower abuse risk than current Schedule 3 drugs, thereby placing it in the same category as propoxyphene.
The FDA issued a drug safety communication in August 2015 alerting health care professionals and the public about a higher risk of respiratory depression in children given tramadol. Then in April 2017 a new warning about the use of codeine and tramadol in children/teens was released. It’s recommended they not be used in people under 12-years-old and the FDA has warned against their use in breastfeeding women. For teens 12-18 years old, the FDA warned against their use in patients with a history of obesity, obstructive sleep apnea, or severe lung disease. Neither should be given to children or adolescents following tonsil or adenoid removal. Paracetamol and NSAIDs are recommended as alternative analgesics.
As of 2016, tramadol was being sold alone or in combination with paracetamol in products from ~90 companies.
USADA science director Matthew Fedoruk says the organization has heard from athletes about tramadol abuse and USADA is now of the opinion that “tramadol abuse threatens athletes’ health and their right to a level playing field.”
A study of young elite cyclists in Italy reported tramadol was commonly considered a doping agent (Loraschi, 2014).
It is said to be the opioid of choice in the Middle East, Northern Africa, and West Africa (Salm-Reifferscheidt, 2018). It is used by workers for its stimulant-like or anti-fatigue effects at lower doses and many people become dependent such that their use is partly driven by the need to avoid withdrawal. It’s a prescription drug in those locations, but it is widely available and cheap outside of medical settings, in part because of a large illicit market that often uses expired or counterfeit pills. Producers, which are frequently located in India or China, have responded to the demand in these regions by raising pill strength to 120, 225, and 250 mg, even though pills usually just contain 50-100 mg.
Thomas Pietschmann, a UNODC drug research expert, noted that the high-strength pills now showing up in the Middle East and Africa don’t make sense from a medical perspective, suggesting they’re being used nonmedically.
Egypt put tramadol under national control, yet in 2015 nearly 70% of people treated at an addiction facility were still using the drug (Salm-Reifferscheidt, 2018). In Nigeria and Benin it’s reportedly mixed with energy drinks for sexual enhancement and it’s prevalent in Gabonese schools, where it’s called “kobolo.”
Attempts to limit its entrance into these countries are limited by relatively porous borders.
In late 2017, the UNODC warned about increasing tramadol trafficking and use. It reported a rise in annual seizures from 300 kg to 3 tonnes since 2013. The major transit or target countries include Benin, Nigeria, Ghana, Togo, Niger, Sierra Leone, Cameroon, and Cote d’Ivoire. Pills tend to originate in South Asia, where they are then trafficked by organized criminal groups to regions of the Sahel that have a notable terrorist presence, with groups like Boko Haram and ISIS. Tramadol trafficking fuels those groups monetarily and fighters frequently consume the drug themselves.
Ghana made an effort to fight tramadol abuse after it increased in 2017.
Olivia Boateng, head of Tobacco and Substances Abuse Department at the Food and Drugs Authority in Ghana:
Tramadol seems to be a factor in violence in Nigeria. A study investigating the link between drug use and conflict in Nigeria revealed many civilians and local leaders/authorities believe tramadol contributes to atrocities on both sides of the conflict between Boko Haram and the Civilian Joint Task Force (CJTF) (Mukpo, 2017). Respondents said it’s commonly used by CJTF members and it’s trafficked within camps for internally displaced people. Aside from cannabis, the most commonly used drugs are tramadol, codeine, and benzhexol. In the Borno region, tramadol was described as playing a role in the conflict with Boko Haram and it was perceived by many to be among the most dangerous drugs in the country.
Marcus Ayuba, the leader of a unit run by the Nigerian National Drug Law Enforcement Agency (NDLEA), says the problem with tramadol is “really huge” and the high rate of use can be tied to a decade of war in the country. In an article published by the BBC, a fighter opposed to Boko Haram described how the drug gives him “strength” to fight, while a Boko Haram fighter described using it the same way. At a port in Lagos, Nigeria, NDLEA authorities broke into a shipping container and discovered millions of tablets in a single shipment. The tablets were branded as “Super RolmeX” and said to contain 225 mg. Supposedly they were manufactured by Sintex Technologies in London, England, yet that company shut down in 2012. The packaging described the tablets as having been made in India.
Rebecca Grant, a national security and military analyst with IRIS Independent Research, says opioid trafficking is a major revenue source for terrorist groups.
A drug shipment seized in 2017 by Italian forces in the port of Genoa in northern Italy contained 37 million tablets hidden under a load of fabrics (Santacroce, 2018). The seized contents were worth €75 million and the tramadol was headed to Libya.
India brought the drug under the control of the Narcotic Drugs and Psychotropic Substances Act in April 2018. This move was in response to its abuse and link to criminal groups.
Evidence from 73 treatment-seeking adolescents and young adults in Sweden indicated tramadol is a commonly used drug in that population (Olsson, 2017). Hair analysis showed it was the most commonly detected opioid. 32% of patients overall tested positive for opioids and in all but one they were positive for tramadol.
A couple studies have shown it’s an adulterant in herbal sexual enhancers sold in Iran (Fard, 2018 ; Dastjerdi, 2018). It’s been detected alongside sildenafil, caffeine, and diazepam, among other drugs.
Langley (2010) reviewed 11 studies on tramadol for osteoarthritis and found the overall rate of adverse events ranged from 45% to 84% with tramadol, compared to 19% to 66% with placebo. The most common adverse effects were GI related (nausea, constipation, vomiting) and CNS-related (dizziness, drowsiness, headache). Two studies found nausea and constipation were significantly more common than with placebo, but neither headache nor vomiting were significantly more common. Most adverse effects appeared in the first four weeks of treatment. Long-acting formulations may reduce the side effect burden.
Adverse effects from therapeutic doses are usually minor or moderate, such as drowsiness, dizziness, headache, nausea, and constipation. It produces a more stable respiratory and hemodynamic profile than classic opioids, minimally affecting vitals at normal doses. Though respiratory depression can be seen, it is less significant than that from classic opioids like morphine or pethidine (Tarkkila, 1998 ; Houmes, 1992). Some studies have failed to show a significant change in respiratory measures. Vickers (1992) reported 0.5 to 2.0 mg/kg IV only caused a non-significant rise in end-tidal CO2, compared to a significant rise from morphine. Overall, there is good evidence that at any of the therapeutic doses, respiration should not be greatly impaired in someone without a preexisting respiratory problem or another risk factor.
At the hemodynamic level, tramadol causes a minor increase or decrease in heart rate and blood pressure. An IV bolus of 100 mg in healthy volunteers caused heart rate to increase by 7 bpm, systolic blood pressure to increase 6 mmHg, and diastolic blood pressure to increase 14 mmHg (Lee, 1993). Whereas 0.75-1.5 mg/kg in children given tramadol postoperatively, the drug caused a decline in heart rate and diastolic blood pressure, but not systolic blood pressure (Lee, 1993).
Tramadol somewhat increases orofecal and colonic transit time, but gastric emptying is not delayed at normal doses, unlike with morphine (Murphy, 1997).
Hypoglycemia occurs at a higher rate in patients receiving tramadol than in patients receiving other opioids (Golightly, 2017). Both MOR agonism and effects on serotonin and norepinephrine can enhance insulin’s effects and promote glucose utilization. The first published case report of hypoglycemia was in 2006 and since then there have been multiple reports showing tramadol sometimes triggers hypoglycemia in both diabetic and non-diabetic people. Blood sugar changes have also been reported in overdose.
Opioids can have a negative effect on immune function; tramadol does not appear as problematic in this regard. Morphine has been shown to reduce natural killer cell activity and T lymphocyte proliferation, whereas tramadol may not impair T lymphocyte function and appears to have a neutral or positive effect on natural killer cell activity (Grond, 2004). Human, animal, and in vitro research has shown less of an effect overall than is seen with typical opioids.
Tramadol overdoses exhibit opioid-like and SNRI-like effects. An overdose from tramadol does not tend to look like a classic CNS depressant overdose, as cardiovascular stimulation may be seen and seizures are fairly common. Respiratory depression and coma are often still reported though and they will likely occur more often in those with efficient or abnormally high O-DSMT production.
Other effects seen in overdose are nausea, vomiting, hyper- or hypoglycemia, sweating, serotonin toxicity symptoms like clonus and hyperthermia, and miosis or mydriasis.
Benzodiazepines and naloxone have been used in the event of overdose to address the SNRI-like and opioid-like effects, respectively. Naloxone significantly improves overdose outcomes and is frequently utilized to symptomatically address symptoms even though it is known to only partially antagonize tramadol (Hussien, 2017). Naloxone is usually able to assist with reversing respiratory depression and coma (Marquardt, 2005). Seizure has been reported after naloxone administration, but that seems to be an atypical response (Spiller, 1997).
Fatalities have occurred but are not common, especially with supportive care.
Serotonin toxicity mostly is not a concern with tramadol-only overdoses. It can occur, but it’s more common when combining it with other serotonergic drugs. At therapeutic doses the combination of tramadol and typical antidepressants, including SSRIs, doesn’t appear to be an issue.
Among the symptoms are agitation, anxiety, disorientating, restlessness, clonus, tremor, hypertension, hyperthermia, tachycardia, tachypnea, vomiting, shivering, mydriasis, and hyperreflexia.
Studies have indicated the toxidrome is connected to 5-HT1A and 5-HT2A activity.
A review of the evidence showed tramadol could be associated with an increased risk of QT interval prolongation and Torsades de pointes (Hancox, 2018). This may primarily occur in overdose rather than in therapeutic use. There is some evidence that tramadol can block Na+ channels at high concentrations, which could explain its ability to alter cardiac function.
Human and animal evidence suggests tramadol and O-DSMT could cause hepatotoxicity. It has only been reported in a small portion of patients and it has also been associated with toxicity in some case reports. Given the low frequency of toxicity reports in the millions of patients using tramadol, therapeutic use may not be a major risk factor for developing liver toxicity.
Fatalities are possible but single-drug toxicity deaths with tramadol are rare. It is most often a problem when high doses are mixed with other CNS depressants or serotonergic drugs. Tramadol-only fatalities tend to show very high concentrations that would not be reached even with common or strong nonmedical doses.
The fatalities on record have included postmortem findings indicative of an opioid-type overdose, suggesting tramadol can fatally inhibit respiratory and cardiac function, at least in some people.
Tramadol has a well-known ability to lower seizure threshold. Seizures have frequently occurred in overdose, though they have also occasionally been reported with therapeutic use of 200-400 mg. It is rare for therapeutic use to produce seizures, but because it is a concern you should discuss the risk with your physician if you are using other seizure threshold-reducing drugs or if you have a history of seizures.
Dependence does exist with prolonged exposure, leading to opioid-like and SNRI-like withdrawal symptoms upon cessation. It can be very uncomfortable in a dose-dependent manner and in a way that is dependent on how fast you stop your use. Those symptoms can be reduced by tapering the drug slowly.
Tolerance also builds over time, leading to reduced effects and a need for higher doses. Analgesic tolerance may build more slowly with tramadol than with other opioids.
Among the potential withdrawal effects are anxiety, depression, sweating, nausea, insomnia, shakiness, confusion, cognitive impairment, aches, rhinorrhea, hallucinations, increased pain, and GI symptoms like diarrhea and stomach pain.
Withdrawal can sometimes last a week or more, but the worst symptoms tend to persist for under five days, especially if the withdrawal is only stemming from therapeutic doses.
Because it does have opioid-like properties mixed with other mechanisms that can improve mood and anxiety, it has been used nonmedically, sometimes producing addiction. Part of the problem with the marketing for tramadol is that it was long described as substantially less risky than other opioids in terms of addiction potential, which led to it being relatively easy to access for a long time and to it being prescribed in cases where a patient had a potentially contraindicated history of drug addiction.
It tends to be less pleasurable than classic opioids, yielding a lower level of euphoria, but it can still be satiating, mood improving, and generally enjoyable (Babalonis, 2013). Because it commonly has a more stimulating/productive quality than classic opioids, it may be easier to build a psychological dependence to the drug without noticing it as clearly. In those who produce more O-DSMT it might be more enjoyable and have a higher chance of being involved in an addiction.
Conditioned place preference (CPP) in animals has been shown, though tramadol is generally regarded as less rewarding in that model (Zhang, 2012). Since the research has tended to involve injections of tramadol via routes that get around first-pass metabolism, that could conceivably contribute to a lower perceived reward potential vs. oral use in humans, considering the likely role of opioid activity from O-DSMT in any rewarding effect of the substance.
There may be a correlation between tramadol use and psychiatric problems, as well as a minor connection with cognitive impairment (Khalifa, 2017 ; Bassiony, 2016). It’s quite possible the psychiatric disorders are not being cause by tramadol and more research is needed to confirm the connection between both issues and tramadol use.
Its effects in pregnancy are not fully understood. It does not appear teratogenic, but it is not clearly safe in all respects (Bloor, 2012). Since tramadol and O-DSMT readily cross the placenta, that should be considered when it’s being used for analgesia in labor. Neonatal abstinence syndrome is a risk when tramadol is used during pregnancy.
Animal research has indicated the potential for memory impairment, neurotoxicity, and organ toxicity (Baghishani, 2018 ; Faria, 2017)
Abdel-Hamid, I. A., Andersson, K.-E., Waldinger, M. D., & Anis, T. H. (2016). Tramadol Abuse and Sexual Function. Sexual Medicine Reviews, 4(3), 235–246. https://doi.org/10.1016/j.sxmr.2015.10.014
Abdel-Zaher, A. O., Abdel-Rahman, M. S., & ELwasei, F. M. (2011). Protective effect of Nigella sativa oil against tramadol-induced tolerance and dependence in mice: Role of nitric oxide and oxidative stress. NeuroToxicology, 32(6), 725–733. https://doi.org/10.1016/j.neuro.2011.08.001
Abel, S. R. (1995). Tramadol: An Alternative Analgesic to Traditional Opioids and NSAIDs. Journal of Pharmaceutical Care in Pain & Symptom Control, 3(1), 5–29. https://doi.org/10.1300/J088v03n01_02
Adams, E. H., Breiner, S., Cicero, T. J., Geller, A., Inciardi, J. A., Schnoll, S. H., … Woody, G. E. (2006). A Comparison of the Abuse Liability of Tramadol, NSAIDs, and Hydrocodone in Patients with Chronic Pain. Journal of Pain and Symptom Management, 31(5), 465–476. https://doi.org/10.1016/j.jpainsymman.2005.10.006
Adams, E. H., & Schnoll, S. H. (2005). Tramadol Abuse and Dependence Among Physicians. JAMA, 293(16), 1977. https://doi.org/10.1001/jama.293.16.1977-a
Afshari, R., & Ghooshkhanehee, H. (2009). Tramadol overdose induced seizure, dramatic rise of CPK and acute renal failure. Journal of the Pakistan Medical Association, 59(3), 178.
Agrawal, A., Diwan, S. K., & Mahajan, R. (2009). Severe delirium following single dose of tramadol. Indian Journal of Medical Sciences, 63(2), 80–1. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19359773
Ahmadi, M., Hoseinzade, A., Haghighi, S., & Yosefi, S. (2017). Complex Partial Seizure and Hippocampus Atrophy Caused by Tramadol Abuse: A Case Study. Annals of Military and Health Sciences Research, 15(1), 4–6. https://doi.org/10.5812/amh.61240
Ahmadimanesh, M., Shadnia, S., Rouini, M. R., Sheikholeslami, B., Ahsani Nasab, S., & Ghazi-Khansari, M. (2018). Correlation between plasma concentrations of tramadol and its metabolites and the incidence of seizure in tramadol-intoxicated patients. Drug Metabolism and Personalized Therapy, 33(2), 75–83. https://doi.org/10.1515/dmpt-2017-0040
Ahmed, M. A., & Kurkar, A. (2014). Effects of opioid (tramadol) treatment on testicular functions in adult male rats: The role of nitric oxide and oxidative stress. Clinical and Experimental Pharmacology and Physiology, 41(4), 317–323. https://doi.org/10.1111/1440-1681.12213
Akbay, B. K., Yildizbas, S., Guclu, E., Yilmaz, S., Iskender, A., & Ozturk, O. (2010). Analgesic efficacy of topical tramadol in the control of postoperative pain in children after tonsillectomy. Journal of Anesthesia, 24(5), 705–8. https://doi.org/10.1007/s00540-010-0978-2
Akkurt, I., Cetin, C., Erdogan, A. M., Dincel, G. C., Ceylan, A. F., Kisa, U., … Bakar, B. (2018). Cerebral ischaemia/reperfusion injury could be managed by using tramadol. Neurological Research, 0(0), 1–11. https://doi.org/10.1080/01616412.2018.1477556
Alghobary, M., El-Bayoumy, Y., Mostafa, Y., Mahmoud, E. H. M., & Amr, M. (2010). Evaluation of tramadol on demand vs. daily paroxetine as a long-term treatment of lifelong premature ejaculation. Journal of Sexual Medicine. https://doi.org/10.1111/j.1743-6109.2010.01789.x
Alinejad, S., Zamani, N., Abdollahi, M., & Mehrpour, O. (2017). A Narrative Review of Acute Adult Poisoning in Iran. Iranian Journal of Medical Sciences, 42(4), 327–346. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/28761199
Aliyu, I., Kyari, F., & Ibrahim, Z. (2016). Hypoglycemia in a child with tramadol poisoning. Saudi Journal of Medicine and Medical Sciences, 4(1), 35. https://doi.org/10.4103/1658-631X.170892
Alizadeh Ghamsari, A., Dadpour, B., & Najari, F. (2016). Frequency of Electrocardiographic Abnormalities in Tramadol Poisoned Patients; a Brief Report. Emergency (Tehran, Iran), 4(3), 151–4. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27299145
Anderson, B. J., Thomas, J., Ottaway, K., & Chalkiadis, G. A. (2017). Tramadol: keep calm and carry on. Pediatric Anesthesia, 27(8), 785–788. https://doi.org/10.1111/pan.13190
Ansermot, N., Chocron, O., Herrera, F., & Eap, C. B. (2015). Severe Manic Episode Associated With Tramadol in a Patient With Recurrent Depressive Disorder. Journal of Clinical Psychopharmacology, 35(2), 203–204. https://doi.org/10.1097/JCP.0000000000000275
Arafa, M. H., & Atteia, H. H. (2018). Genetic polymorphisms of cytochrome P450 2D6 (CYP2D6) are associated with long term tramadol treatment-induced oxidative damage and hepatotoxicity. Toxicology and Applied Pharmacology (Vol. 346). Elsevier Inc. https://doi.org/10.1016/j.taap.2018.03.019
Asadi, P., Monsef Kasmaei, V., Ziabari, S. Z., Zohrevandi, B., & Moadab Manesh, A. (2015). Prevalence of Tramadol Consumption in First Seizure Patients; a One-Year Cross-sectional Study. Emergency (Tehran, Iran), 3(4), 159–61. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4608351&tool=pmcentrez&rendertype=abstract
Asari, Y., Ikeda, Y., Tateno, A., Okubo, Y., Iijima, T., & Suzuki, H. (2018). Acute tramadol enhances brain activity associated with reward anticipation in the nucleus accumbens. Psychopharmacology, 1–12. https://doi.org/10.1007/s00213-018-4955-z
Asghari, A., Akbari, G., Beigi, A. M., & Mortazavi, P. (2016). Tramadol reduces testicular damage of ischemia-reperfusion rats. Animal Reproduction, 13(4), 811–819. https://doi.org/10.21451/1984-3143-AR823
Aslan-Tutak, F., & Adams, T. L. (2015). A study of geometry content knowledge of elementary preservice teachers. International Electronic Journal of Elementary Education, 7(3), 301–318. https://doi.org/10.1007/s
ATICI, S., CINEL, L., CINEL, I., DORUK, N., AKTEKIN, M., AKCA, A., … ORAL, U. (2004). OPIOID NEUROTOXICITY: COMPARISON OF MORPHINE AND TRAMADOL IN AN EXPERIMENTAL RAT MODEL. International Journal of Neuroscience, 114(8), 1001–1011. https://doi.org/10.1080/00207450490461314
Axiak-Bechtel, S. M., Tsuruta, K., Amorim, J., Donaldson, R., Lino, G., Honaker, A., … Declue, A. (2015). Effects of tramadol and o-desmethyltramadol on canine innate immune system function. Veterinary Anaesthesia and Analgesia, 42(3), 260–268. https://doi.org/10.1111/vaa.12201
Babalonis, S., Lofwall, M. R., Nuzzo, P. A., Siegel, A. J., & Walsh, S. L. (2013). Abuse liability and reinforcing efficacy of oral tramadol in humans. Drug and Alcohol Dependence, 129(1–2), 116–124. https://doi.org/10.1016/j.drugalcdep.2012.09.018
Bachs, L. C., Engeland, A., Mørland, J. G., & Skurtveit, S. (2009). The risk of motor vehicle accidents involving drivers with prescriptions for codeine or tramadol. Clinical Pharmacology and Therapeutics, 85(6), 596–599. https://doi.org/10.1038/clpt.2009.14
Baghishani, F., Mohammadipour, A., Hosseinzadeh, H., Hosseini, M., & Ebrahimzadeh-bideskan, A. (2018). The effects of tramadol administration on hippocampal cell apoptosis, learning and memory in adult rats and neuroprotective effects of crocin. Metabolic Brain Disease, 33(3), 907–916. https://doi.org/10.1007/s11011-018-0194-6
Bameri, B., Shaki, F., Ahangar, N., Ataee, R., Samadi, M., & Mohammadi, H. (2018). Evidence for the Involvement of the Dopaminergic System in Seizure and Oxidative Damage Induced by Tramadol. International Journal of Toxicology, 37(2), 164–170. https://doi.org/10.1177/1091581817753607
Bamigbade, T. ., & et al. (1997). Actions of Tramadol, its enantiomers and principle metabolyte, O-desmethyltramadol on serotonin (5-HT) efflux and uptake in rat dorsal raphe nucleus. British Journal of Anaesthetics, 79, 352–356.
Bar-Or, D., Salottolo, K. M., Orlando, A., & Winkler, J. V. (2012). A randomized double-blind, placebo-controlled multicenter study to evaluate the efficacy and safety of two doses of the tramadol orally disintegrating tablet for the treatment of premature ejaculation within less than 2 minutes. European Urology, 61(4), 736–743. https://doi.org/10.1016/j.eururo.2011.08.039
Barann, M., Stamer, U. M., Lyutenska, M., Stüber, F., Bönisch, H., & Urban, B. (2014). Effects of opioids on human serotonin transporters. Naunyn-Schmiedeberg’s Archives of Pharmacology, 388(1), 43–49. https://doi.org/10.1007/s00210-014-1056-3
Barber, J. (2011). Examining the Use of Tramadol Hydrochloride as an Antidepressant. Experimental and Clinical Psychopharmacology, 19(2), 123–130. https://doi.org/10.1037/a0022721
Barbera, N., Fisichella, M., Bosco, A., Indorato, F., Spadaro, G., & Romano, G. (2013). A suicidal poisoning due to tramadol. A metabolic approach to death investigation. Journal of Forensic and Legal Medicine, 20(5), 555–558. https://doi.org/10.1016/j.jflm.2013.03.006
Barnung, K. S., Treschow, M., & Borgbjerg, M. F. (1997). Respiratory depression following oral tramadol in a patient with impaired renal function. Pain, 71(1), 111–112. https://doi.org/10.1016/S0304-3959(97)03350-2
Barsotti, C. E., Mycyk, M. B., & Reyes, J. (2003). Withdrawal syndrome from tramadol hydrochloride [3]. American Journal of Emergency Medicine, 21(1), 87–88. https://doi.org/10.1053/ajem.2003.50039
Bassiony, M. M., Salah El-Deen, G. M., Yousef, U., Raya, Y., Abdel-Ghani, M. M., El-Gohari, H., & Atwa, S. A. (2015). Adolescent tramadol use and abuse in Egypt. American Journal of Drug and Alcohol Abuse, 41(3), 206–211. https://doi.org/10.3109/00952990.2015.1014959
Bassiony, M. M., Youssif, U. M., Hussein, R. A., & Saeed, M. (2016). Psychiatric Comorbidity Among Egyptian Patients With Opioid Use Disorders Attributed to Tramadol. Journal of Addiction Medicine, 10(4), 262–268. https://doi.org/10.1097/ADM.0000000000000231
Beakley, B. D., Kaye, A. M., & Kaye, A. D. (2015). Tramadol, Pharmacology, Side Effects, and Serotonin Syndrome: A Review. Pain Physician, 18(4), 395–400. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26218943
Belin, N., Clairet, A.-L., Chocron, S., Capellier, G., & Piton, G. (2017). Refractory Cardiogenic Shock During Tramadol Poisoning: A Case Report. Cardiovascular Toxicology, 17(2), 219–222. https://doi.org/10.1007/s12012-016-9373-z
Bennett, R. M., Kamin, M., Karim, R., & Rosenthal, N. (2003). Tramadol and acetaminophen combination tablets in the treatment of fibromyalgia pain: A double-blind, randomized, placebo-controlled study. American Journal of Medicine, 114(7), 537–545. https://doi.org/10.1016/S0002-9343(03)00116-5
Berrocoso, E., Rojas-Corrales, M. O., & Mico, J. A. (2006). Differential role of 5-HT1A and 5-HT1B receptors on the antinociceptive and antidepressant effect of tramadol in mice. Psychopharmacology, 188(1), 111–118. https://doi.org/10.1007/s00213-006-0464-6
Bilir, A., Erkasap, N., Koken, T., Gulec, S., Kaygisiz, Z., Tanriverdi, B., & Kurt, I. (2007). Effects of tramadol on myocardial ischemia-reperfusion injury. Scandinavian Cardiovascular Journal, 41(4), 242–247. https://doi.org/10.1080/14017430701227747
Biswas, S., Chandanwale, A. S., Sundar, S., Gabhane, M., Naik, M., Patel, K., & Latchoumibady, V. (2014). Efficacy and safety profile of combination of tramadol-diclofenac versus tramadol-paracetamol in patients with acute musculoskeletal conditions, postoperative pain, and acute flare of osteoarthritis and rheumatoid arthritis: a Phase III, 5-day open-label. Journal of Pain Research, 26(S1), 455. https://doi.org/10.2147/JPR.S67817
Bloms-Funke, P., Dremencov, E., Cremers, T. I. F. H., & Tzschentke, T. M. (2011). Tramadol increases extracellular levels of serotonin and noradrenaline as measured by in vivo microdialysis in the ventral hippocampus of freely-moving rats. Neuroscience Letters, 490(3), 191–195. https://doi.org/10.1016/j.neulet.2010.12.049
Bloor, M., Paech, M. J., & Kaye, R. (2012). Tramadol in pregnancy and lactation. International Journal of Obstetric Anesthesia, 21(2), 163–167. https://doi.org/10.1016/j.ijoa.2011.10.008
Bosenberg, A. T., & Ratcliffe, S. (1998). The respiratory effects of tramadol in children under halothane anaesthesia. Anaesthesia, 53(10), 960–964. https://doi.org/10.1046/j.1365-2044.1998.00526.x
Boumendjel, A., Sotoing-Ta??we, G., Ngo-Bum, E., Chabrol, T., Beney, C., Sinniger, V., … De-Waard, M. (2013). Occurrence of the synthetic analgesic tramadol in an African medicinal plant. Angewandte Chemie – International Edition, 52(45), 11780–11784. https://doi.org/10.1002/anie.201305697
Boureau, F., Legallicier, P., & Kabir-Ahmadi, M. (2003). Tramadol in post-herpetic neuralgia: A randomized, double-blind, placebo-controlled trial. Pain, 104(1–2), 323–331. https://doi.org/10.1016/S0304-3959(03)00020-4
Bourne, C., Gouraud, A., Daveluy, A., Grandvuillemin, A., Auriche, P., Descotes, J., & Vial, T. (2013). Tramadol and hypoglycaemia: Comparison with other step 2 analgesic drugs. British Journal of Clinical Pharmacology, 75(4), 1063–1067. https://doi.org/10.1111/j.1365-2125.2012.04451.x
Bravo, L., Mico, J. A., & Berrocoso, E. (2017). Discovery and development of tramadol for the treatment of pain. Expert Opinion on Drug Discovery, 12(12), 1281–1291. https://doi.org/10.1080/17460441.2017.1377697
Brouquet, A., Cudennec, T., Benoist, S., Moulias, S., Beauchet, A., Penna, C., … Nordlinger, B. (2010). Impaired mobility, ASA status and administration of tramadol are risk factors for postoperative delirium in patients aged 75 years or more after major abdominal surgery. Annals of Surgery, 251(4), 759–765. https://doi.org/10.1097/SLA.0b013e3181c1cfc9
Bush, D. M. (2013). Emergency Department Visits for Drug Misuse or Abuse Involving the Pain Medication Tramadol. The CBHSQ Report. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26913326
But, A. K., Erdil, F., Yucel, A., Gedik, E., Durmus, M., & Ersoy, M. O. (2007). The effects of single-dose tramadol on post-operative pain and morphine requirements after coronary artery bypass surgery. Acta Anaesthesiologica Scandinavica, 51(5), 601–606. https://doi.org/10.1111/j.1399-6576.2007.01275.x
C.A., O. (2016). What’s tramadol got to do with it? A case report of rebound hypoglycemia, a reappraisal and review of potential mechanisms. Pain Physician, 19(8), E1215–E1220. Retrieved from http://www.painphysicianjournal.com/current/pdf?article=MzEyMg%3D%3D%0Ahttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed18&NEWS=N&AN=613555220
Cami J, Lamas X, F. M. (1994). Acute effects of tramadol in metha- done-maintained volunteers. Drugs, 47(1), 39–43.
Campbell, W. I., Kendrick, R. W., Ramsay-Baggs, P., & McCaughey, W. (1997). The effect of pre-operative administration of bupivacaine compared with its postoperative use. Anaesthesia, 52(12), 1212–1216. https://doi.org/10.1111/j.1365-2044.1997.219-az0353.x
Candeletti, S., Lopetuso, G., Cannarsa, R., Cavina, C., & Romualdi, P. (2006). Effects of Prolonged Treatment With the Opiate Tramadol on Prodynorphin Gene Expression in Rat CNS. Journal of Molecular Neuroscience, 30(3), 341–348. https://doi.org/10.1385/JMN:30:3:341
Caspani, O., Reitz, M. C., Ceci, A., Kremer, A., & Treede, R. D. (2014). Tramadol reduces anxiety-related and depression-associated behaviors presumably induced by pain in the chronic constriction injury model of neuropathic pain in rats. Pharmacology Biochemistry and Behavior, 124, 290–296. https://doi.org/10.1016/j.pbb.2014.06.018
Cepeda, M. S., Camargo, F., Zea, C., & Valencia, L. (2006). Tramadol for osteoarthritis. Cochrane Database of Systematic Reviews, (3). https://doi.org/10.1002/14651858.CD005522.pub2
Ceylan, D., Kaçar, M., & Ulaş, H. (2015). Manic Episodes Associated With Tramadol. Journal of Clinical Psychopharmacology, 35(1), 111–113. https://doi.org/10.1097/JCP.0000000000000231
Chand, P., Jayaram, N., & Murthy, P. (2017). Iatrogenic tramadol addiction. Indian Journal of Medical Sciences, 69(1), 57. https://doi.org/10.18203/issn.0019-5359.IndianJMedSci20170495
Chaparro, L. E., Furlan, A. D., Deshpande, A., Mailis-Gagnon, A., Atlas, S., & Turk, D. C. (2014). Opioids Compared With Placebo or Other Treatments for Chronic Low Back Pain. Spine, 39(7), 556–563. https://doi.org/10.1097/BRS.0000000000000249
Chen, K. J., Lu, M. L., & Shen, W. W. (2015). Tramadol-related psychosis in a patient with bipolar i disorder. Acta Neuropsychiatrica, 27(2), 126–128. https://doi.org/10.1017/neu.2014.45
Chen, T. C., Chen, L. C., & Knaggs, R. D. (2018). A 15-year overview of increasing tramadol utilisation and associated mortality and the impact of tramadol classification in the United Kingdom. Pharmacoepidemiology and Drug Safety. https://doi.org/10.1002/pds.4320
Chew, S. T. H., Ip-Yam, P. C., & Kong, C. F. (2003). Recovery following tonsillectomy a comparison between tramadol and morphine for analgesia. Singapore Medical Journal, 44(6), 296–8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/14560861
Choi, C. B., Song, J. S., Kang, Y. M., Suh, C. H., Lee, J., Choe, J. Y., … Bae, S. C. (2007). A 2-Week, multicenter, randomized, double-blind, double-dummy, add-on study of the effects of titration on tolerability of tramadol/acetaminophen combination tablet in Korean adults with knee osteoarthritis pain. Clinical Therapeutics, 29(7), 1381–1389. https://doi.org/10.1016/j.clinthera.2007.07.015
Cicero, T. J., Adams, E. H., Geller, A., Inciardi, J. A., Munoz, A., Schnoll, S. H., … Woody, G. E. (1999). A postmarketing surveillance program to monitor Ultram (R) (tramadol hydrochloride) abuse in the United States. Drug and Alcohol Dependence, 57(1), 7–22. https://doi.org/10.1016/s0376-8716(99)00041-1
Cicero, T. J., Inciardi, J. A., Adams, E. H., Geller, A., Senay, E. C., Woody, G. E., & Muñoz, A. (2005). Rates of abuse of tramadol remain unchanged with the introduction of new branded and generic products: results of an abuse monitoring system, 1994-2004. Pharmacoepidemiology and Drug Safety, 14(12), 851–859. https://doi.org/10.1002/pds.1113
Clarot, F., Goullé, J. P., Vaz, E., & Proust, B. (2003). Fatal overdoses of tramadol: Is benzodiazepine a risk factor of lethality? Forensic Science International, 134(1), 57–61. https://doi.org/10.1016/S0379-0738(03)00100-2
Coller, J. K., Michalakas, J. R., James, H. M., Farquharson, A. L., Colvill, J., White, J. M., & Somogyi, A. A. (2012). Inhibition of CYP2D6-mediated tramadol O-demethylation in methadone but not buprenorphine maintenance patients. British Journal of Clinical Pharmacology. https://doi.org/10.1111/j.1365-2125.2012.04256.x
Dal, D., Salman, M. A., Salman, A. E., Iskit, A. B., & Aypar, Ü. (2006). The involvement of nitric oxide on the analgesic effect of tramadol. European Journal of Anaesthesiology, 23(2), 175–177. https://doi.org/10.1017/S0265021505222111
Dastjerdi, A. G., Akhgari, M., Kamali, A., & Mousavi, Z. (2018). Principal component analysis of synthetic adulterants in herbal supplements advertised as weight loss drugs. Complementary Therapies in Clinical Practice, 31, 236–241. https://doi.org/10.1016/j.ctcp.2018.03.007
Daubin, C., Quentin, C., Goullé, J.-P., Guillotin, D., Lehoux, P., Lepage, O., & Charbonneau, P. (2007). Refractory shock and asystole related to tramadol overdose. Clinical Toxicology, 45(8), 961–964. https://doi.org/10.1080/15563650701438847
Dayer, P., Collart, L., & Desmeules, J. (1994). The Pharmacology of Tramadol. Drugs, 47(Supplement 1), 3–7. https://doi.org/10.2165/00003495-199400471-00003
De Backer, B., Renardy, F., Denooz, R., & Charlier, C. (2010). Quantification in postmortem blood and identification in urine of tramadol and its two main metabolites in two cases of lethal tramadol intoxication. Journal of Analytical Toxicology, 34(9), 599–604. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21073815
De Decker, K., Cordonnier, J., Jacobs, W., Coucke, V., Schepens, P., & Jorens, P. G. (2008). Fatal intoxication due to tramadol alone. Case report and review of the literature. Forensic Science International, 175(1), 79–82. https://doi.org/10.1016/j.forsciint.2007.07.010
De Witte, J., Deloof, T., De Veylder, J., & Housmans, P. R. (1997). Tramadol in the treatment of postanesthetic shivering. Acta Anaesthesiol Scand, 41, 506–510.
De Witte, J. L., Schoenmaekers, B., Sessler, D. I., & Deloof, T. (2001). The analgesic efficacy of tramadol is impaired by concurrent administration of ondansetron. Anesthesia and Analgesia, 92(5), 1319–21. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11323369
Debono, M., Chan, S., Rolfe, C., & Jones, T. H. (2011). Tramadol-induced adrenal insufficiency. European Journal of Clinical Pharmacology, 67(8), 865–867. https://doi.org/10.1007/s00228-011-0992-9
Delilkan, A. E., & Vijayan, R. (1993). Epidural tramadol for postoperative pain relief. Anaesthesia, 48(4), 328–31. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8494137
Derry, S., Cooper, T. E., & Phillips, T. (2016). Single fixed-dose oral dexketoprofen plus tramadol for acute postoperative pain in adults. Cochrane Database of Systematic Reviews, 2016(9). https://doi.org/10.1002/14651858.CD012232.pub2
Desmeules, J. A., Piguet, V., Collart, L., & Dayer, P. (1996). Contribution of monoaminergic modulation to the analgesic effect of tramadol. British Journal of Clinical Pharmacology, 41(1), 7–12. https://doi.org/10.1111/j.1365-2125.1996.tb00152.x
Dion, G. R., Teng, S. E., Achlatis, E., Fang, Y., & Amin, M. R. (2017). Treatment of Neurogenic Cough with Tramadol: A Pilot Study. Otolaryngology – Head and Neck Surgery (United States), 157(1), 77–79. https://doi.org/10.1177/0194599817703949
Driessen, B., Reimann, W., & Giertz, H. (1993). Effects of the central analgesic tramadol on the uptake and release of noradrenaline and dopamine in vitro. British Journal of Pharmacology, 108(3), 806–811. https://doi.org/10.1111/j.1476-5381.1993.tb12882.x
Duehmke, R. M., Derry, S., Wiffen, P. J., Bell, R. F., Aldington, D., & Moore, R. A. (2017). Tramadol for neuropathic pain in adults. Cochrane Database of Systematic Reviews, 6(6), 1–51. https://doi.org/10.1002/14651858.CD003726.pub4
Duke, A. N., Bigelow, G. E., Lanier, R. K., & Strain, E. C. (2011). Discriminative stimulus effects of tramadol in humans. The Journal of Pharmacology and Experimental Therapeutics, 338(1), 255–62. https://doi.org/10.1124/jpet.111.181131
Dunn, K. E., Tompkins, D. A., Bigelow, G., & Strain, E. C. (2017). Randomized controlled evaluation of tramadol for opioid detoxification. Drug and Alcohol Dependence, 171(2017), e57. https://doi.org/10.1016/j.drugalcdep.2016.08.168
Dunn, K. E., Tompkins, D. A., & Strain, E. C. (2018). Tramadol Extended-Release and Opioid Withdrawal Management—Legal Implications—Reply. JAMA Psychiatry, 75(2), 215. https://doi.org/10.1001/jamapsychiatry.2017.3827
Edwards, J. E., McQuay, H. J., & Moore, R. A. (2002). Combination analgesic efficacy: Individual patient data meta-analysis of single-dose oral tramadol plus acetaminophen in acute postoperative pain. Journal of Pain and Symptom Management, 23(2), 121–130. https://doi.org/10.1016/S0885-3924(01)00404-3
El-Hadidy, M. A., & Helaly, A. M. N. (2015). Medical and psychiatric effects of long-term dependence on high dose of tramadol. Substance Use and Misuse, 50(5), 582–589. https://doi.org/10.3109/10826084.2014.991406
Elkalioubie, A., Allorge, D., Robriquet, L., Wiart, J. F., Garat, A., Broly, F., & Fourrier, F. (2011). Near-fatal tramadol cardiotoxicity in a CYP2D6 ultrarapid metabolizer. European Journal of Clinical Pharmacology, 67(8), 855–858. https://doi.org/10.1007/s00228-011-1080-x
Elmanama, A. A., Abu Tayyem, N. E. S., Essawaf, H. N., & Hmaid, I. M. (2015). Tramadol-Induced Liver and Kidney Toxicity among Abusers in Gaza Strip , Palestine. Jordan Journal of Biological Sciences, 8(2), 133–37. https://doi.org/10.12816/0027559
Emamhadi, M., Sanaei-Zadeh, H., Nikniya, M., Zamani, N., & Dart, R. C. (2012). Electrocardiographic manifestations of tramadol toxicity with special reference to their ability for prediction of seizures. American Journal of Emergency Medicine, 30(8), 1481–1485. https://doi.org/10.1016/j.ajem.2011.12.009
Engelhardt, T., Steel, E., Johnston, G., & Veitch, D. Y. (2003). Tramadol for pain relief in children undergoing tonsillectomy: a comparison with morphine. Paediatric Anaesthesia, 13(3), 249–52. https://doi.org/10.1097/MLG.0b013e318178272e
Epstein, D. H., Preston, K. L., & Jasinski, D. R. (2006). Abuse liability, behavioral pharmacology, and physical-dependence potential of opioids in humans and laboratory animals: Lessons from tramadol. Biological Psychology, 73(1), 90–99. https://doi.org/10.1016/j.biopsycho.2006.01.010
Farajidana, H., Hassanian-Moghaddam, H., Zamani, N., & Sanaei-Zadeh, H. (2012). Tramadol-induced seizures and trauma. European Review for Medical and Pharmacological Sciences, 16(SUPPL. 1), 34–37.
Fard. (2018). Analytical perspectives of chemical adulterants in herbal sexual enhancer drugs, (January).
Faria, J., Barbosa, J., Leal, S., Afonso, L. P., Lobo, J., Moreira, R., … Dinis-Oliveira, R. J. (2017). Effective analgesic doses of tramadol or tapentadol induce brain, lung and heart toxicity in Wistar rats. Toxicology, 385, 38–47. https://doi.org/10.1016/j.tox.2017.05.003
Faria, J., Barbosa, J., Moreira, R., Queirós, O., Carvalho, F., & Dinis-Oliveira, R. J. (2018). Comparative pharmacology and toxicology of tramadol and tapentadol. European Journal of Pain, 22(5), 827–844. https://doi.org/10.1002/ejp.1196
Finnerup, N. B., Attal, N., Haroutounian, S., McNicol, E., Baron, R., Dworkin, R. H., … Wallace, M. (2015). Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. The Lancet Neurology, 14(2), 162–173. https://doi.org/10.1016/S1474-4422(14)70251-0
Flôr, P. B., Yazbek, K. V., Ida, K. K., & Fantoni, D. T. (2013). Tramadol plus metamizole combined or not with anti-inflammatory drugs is clinically effective for moderate to severe chronic pain treatment in cancer patients. Veterinary Anaesthesia and Analgesia, 40(3), 316–327. https://doi.org/10.1111/vaa.12023
Fournier, J.-P., Azoulay, L., Yin, H., Montastruc, J.-L., & Suissa, S. (2015). Tramadol Use and the Risk of Hospitalization for Hypoglycemia in Patients With Noncancer Pain. JAMA Internal Medicine, 175(2), 186. https://doi.org/10.1001/jamainternmed.2014.6512
Freye, E., & Levy, J. (2000). Acute abstinence syndrome following abrupt cessation of long-term use of tramadol (Ultram®): A case study. European Journal of Pain. https://doi.org/10.1053/eujp.2000.0187
Fujimoto, Y., Funao, T., Suehiro, K., Takahashi, R., Mori, T., & Nishikawa, K. (2015). Brain Serotonin Content Regulates the Manifestation of Tramadol-induced Seizures in Rats. Anesthesiology, 122(1), 178–189. https://doi.org/10.1097/ALN.0000000000000434
Gan, S. H., Ismail, R., Wan Adnan, W. A., & Zulmi, W. (2007). Impact of CYP2D6 genetic polymorphism on tramadol pharmacokinetics and pharmacodynamics. Molecular Diagnosis & Therapy, 11(3), 171–181. https://doi.org/10.1007/BF03256239
Garret, P. M. (2004). Tramadol overdose and serotonin syndrome manifesting as acute right heart dysfunction. Anaesthesia and Intensive Care.
Garrido, M. J., Valle, M., Campanero, M. a, Calvo, R., & Trocóniz, I. F. (2000). Modeling of the in vivo antinociceptive interaction between an opioid agonist, (+)-O-desmethyltramadol, and a monoamine reuptake inhibitor, (-)-O-desmethyltramadol, in rats. The Journal of Pharmacology and Experimental Therapeutics, 295(1), 352–9. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10992001
Geracioti, T. D. (2014). Tramadol treatment of combat-related posttraumatic stress disorder. Annals of Clinical Psychiatry : Official Journal of the American Academy of Clinical Psychiatrists, 26(3), 217–221.
Ghazimirsaeid, S. A., Khakzad, M., Dinpanah, H., Amani, N., Rahimi, M., & Manuchehri, A. A. (2014). Tramadol, seizure caused by an overdose and acute renal failure: A case report. World Applied Sciences Journal, 32(7), 1204–1208. https://doi.org/10.5829/idosi.wasj.2014.32.07.1252
Gheshlaghi, F., Eizadi-mood, N., Fazel, K., & Behjati, M. (2009). An unexpected sudden death by oral tramadol intoxication : a case not, 2(4), 292–294.
Gibbison, B., Bailey, C. R., & Klein, A. A. (2015). Tramadol – the Marmite TM drug. Anaesthesia, 70(2), 125–130. https://doi.org/10.1111/anae.12972
Gillen, C., Haurand, M., Kobelt, D. J., & Wnendt, S. (2000). Affinity, potency and efficacy of tramadol and its metabolites at the cloned human μ-opioid receptor. Naunyn-Schmiedeberg’s Archives of Pharmacology, 362(2), 116–121. https://doi.org/10.1007/s002100000266
Gioia, S., Lancia, M., Bacci, M., & Suadoni, F. (2017). Two Fatal Intoxications Due to Tramadol Alone. The American Journal of Forensic Medicine and Pathology, 0(0), 1. https://doi.org/10.1097/PAF.0000000000000338
Golightly, L. K., Simendinger, B. A., Barber, G. R., Stolpman, N. M., Kick, S. D., & McDermott, M. T. (2017). Hypoglycemic effects of tramadol analgesia in hospitalized patients: A case-control study. Journal of Diabetes and Metabolic Disorders, 16(1), 1–9. https://doi.org/10.1186/s40200-017-0311-9
Goodarzi, F., Mehrpour, O., & Eizadi-Mood, N. (2011). A study to evaluate factors associated with seizure in tramadol poisoning in Iran. Indian Journal of Forensic Medicine and Toxicology, 5(2), 66–69.
Grace, D., & Fee, J. P. (1995). Ineffective analgesia after extradural tramadol hydrochloride in patients undergoing total knee replacement. Anaesthesia, 50(6), 555–558.
Grond, S., & Sablotzki, A. (2004). Clinical pharmacology of tramadol. Clinical Pharmacokinetics, 43(13), 879–923. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15509185
Haeseler, G., Foadi, N., Ahrens, J., Dengler, R., Hecker, H., & Leuwer, M. (2006). Tramadol, fentanyl and sufentanil but not morphine block voltage-operated sodium channels. Pain, 126(1–3), 234–244. https://doi.org/10.1016/j.pain.2006.07.003
Hancox, J. (2018). Tramadol linked QT interval prolongation and Torsades de pointes. Annals of Cardiology and Vascular Medicine Open, 7–9.
Hara, K., Minami, K., & Sata, T. (2005). The Effects of Tramadol and Its Metabolite on Glycine, ??-Aminobutyric AcidA, and N-Methyl-d-Aspartate Receptors Expressed in Xenopus Oocytes. Anesthesia & Analgesia, 100(5), 1400–1405. https://doi.org/10.1213/01.ANE.0000150961.24747.98
Harati, Y., Gooch, C., Swenson, M., Edelman, S., Greene, D., Raskin, P., … Kamin, M. (1998). Double-blind randomized trial of tramadol for the treatment of the pain of diabetic neuropathy. Neurology, 50(6), 1842–6. https://doi.org/10.1212/WNL.50.6.1842 This
Harati, Y., Gooch, C., Swenson, M., Edelman, S. V., Greene, D., Raskin, P., … Kamin, M. (2000). Maintenance of the long-term effectiveness of tramadol in treatment of the pain of diabetic neuropathy. Journal of Diabetes and Its Complications, 14(2), 65–70. https://doi.org/10.1016/S1056-8727(00)00060-X
Hassanian-Moghaddam, H., Farajidana, H., Sarjami, S., & Owliaey, H. (2013). Tramadol-induced apnea. American Journal of Emergency Medicine, 31(1), 26–31. https://doi.org/10.1016/j.ajem.2012.05.013
Hassanian-Moghaddam, H., Farnaghi, F., & Rahimi, M. (2015). Tramadol overdose and apnea in hospitalized children, a review of 20 cases. Research in Pharmaceutical Sciences, 10(6), 544–52. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26779274
Houlihan, D. J. (2004). Serotonin Syndrome Resulting from Coadministration of Tramadol, Venlafaxine, and Mirtazapine. Annals of Pharmacotherapy, 38(3), 411–413. https://doi.org/10.1345/aph.1D344
Houmes, R. J., Voets, M. A., Verkaaik, A., Erdmann, W., & Lachmann, B. (1992). Efficacy and safety of tramadol versus morphine for moderate and severe postoperative pain with special regard to respiratory depression. Anesthesia and Analgesia, 74(4), 510–4. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1554117
Hull, M. J., Griggs, D., Knoepp, S. M., Smogorzewska, A., Nixon, A., & Flood, J. G. (2006). Postmortem urine immunoassay showing false-positive phencyclidine reactivity in a case of fatal tramadol overdose. American Journal of Forensic Medicine and Pathology, 27(4), 359–362. https://doi.org/10.1097/01.paf.0000233534.59330.c2
Hussien, R., & Khairat Elguindy, M. (2017). Assessment of the Role of Naloxone in the Prognosis of Tramadol Intoxicated Patients. Journal of Clinical Toxicology, 7(6). https://doi.org/10.4172/2161-0495.1000366
Ide, S., Minami, M., Ishihara, K., Uhl, G. R., Sora, I., & Ikeda, K. (2006). Mu opioid receptor-dependent and independent components in effects of tramadol. Neuropharmacology, 51(3), 651–658. https://doi.org/10.1016/j.neuropharm.2006.05.008
Inciardi, J. A., Cicero, T. J., Muñoz, A., Adams, E. H., Geller, A., Senay, E. C., & Woody, G. E. (2006). The Diversion of Ultram®, Ultracet®, and Generic Tramadol HCl. Journal of Addictive Diseases, 25(2), 53–58. https://doi.org/10.1300/J069v25n02_08
Iravani, F. S., Akhgari, M., Jokar, F., & Bahmanabadi, L. (2010). Current trends in tramadol-related fatalities, Tehran, Iran 20052008. Substance Use and Misuse, 45(13), 2162–2171. https://doi.org/10.3109/10826081003692098
Isiordia-Espinoza, M. A., De Jesús Pozos-Guillén, A., & Aragon-Martinez, O. H. (2014). Analgesic efficacy and safety of single-dose tramadol and non-steroidal anti-inflammatory drugs in operations on the third molars: A systematic review and meta-analysis. British Journal of Oral and Maxillofacial Surgery, 52(9), 775–783. https://doi.org/10.1016/j.bjoms.2014.05.005
Iyer, S., Mohan, G., Ramakrishnan, S., & Theodore, S. (2015). Comparison of tapentadol with tramadol for analgesia after cardiac surgery. Annals of Cardiac Anaesthesia, 18(3), 352. https://doi.org/10.4103/0971-9784.159805
Jafari-Sabet, M., Jafari-Sabet, A. R., & Dizaji-Ghadim, A. (2016). Tramadol state-dependent memory: Involvement of dorsal hippocampal muscarinic acetylcholine receptors. Behavioural Pharmacology, 27(5), 470–478. https://doi.org/10.1097/FBP.0000000000000239
Jesse, C. R., Wilhelm, E. A., Bortolatto, C. F., & Nogueira, C. W. (2010). Evidence for the involvement of the noradrenergic system, dopaminergic and imidazoline receptors in the antidepressant-like effect of tramadol in mice. Pharmacology Biochemistry and Behavior, 95(3), 344–350. https://doi.org/10.1016/j.pbb.2010.02.011
Jin, J. (2017). Risks of Codeine and Tramadol in Children. JAMA, 318(15), 1514. https://doi.org/10.1001/jama.2017.13534
Jovanović-Čupić, V., Martinović, Ž., & Nešić, N. (2006). Seizures Associated with Intoxication and Abuse of Tramadol. Clinical Toxicology, 44(2), 143–146. https://doi.org/10.1080/1556365050014418
Kampe, S., Wolter, K., Warm, M., Dagtekin, O., Shaheen, S., & Landwehr, S. (2009). Clinical equivalence of controlled-release oxycodone 20 mg and controlled-release tramadol 200 mg after surgery for breast cancer. Pharmacology, 84(5), 276–281. https://doi.org/10.1159/000242998
Kaneko, K., Umehara, M., Homan, T., Okamoto, K., Oka, M., & Oyama, T. (2014). The analgesic effect of tramadol in animal models of neuropathic pain and fibromyalgia. Neuroscience Letters, 562, 28–33. https://doi.org/10.1016/j.neulet.2014.01.007
Kapral, S., Gollmann, G., Waltl, B., Likar, R., Sladen, R. N., Weinstabl, C., & Lehofer, F. (1999). Tramadol Added to Mepivacaine Prolongs the Duration of an Axillary Brachial Plexus Blockade. Anesthesia & Analgesia, 88(4), 853–856. https://doi.org/10.1213/00000539-199904000-00032
Karabayirli, S., Ayrm, A. A., & Muslu, B. (2012). Comparison of the Analgesic Effects of Oral Tramadol and Naproxen Sodium on Pain Relief During IUD Insertion. Journal of Minimally Invasive Gynecology, 19(5), 581–584. https://doi.org/10.1016/j.jmig.2012.04.004
Kargi, E., Babuccu, O., Altunkaya, H., Hosnuter, M., Ozer, Y., Babuccu, B., & Payasli, C. (2008). Tramadol as a local anaesthetic in tendon repair surgery of the hand. J Int Med Res, 36, 971–978. Retrieved from internal-pdf://142.0.15.51/Kargi-2008-Tramadol as a local.pdf%5Cnhttp://imr.sagepub.com/content/36/5/971.full.pdf
Katsarava, Z., & Limmroth, V. (2006). Is a combination of tramadol and acetaminophen effective for the treatment of acute migraine pain? Nature Clinical Practice Neurology, 2(7), 360–361. https://doi.org/10.1038/ncpneuro0223
Kaynar, M., Kilic, O., & Yurdakul, T. (2012). On-demand tramadol hydrochloride use in premature ejaculation treatment. Urology, 79(1), 145–149. https://doi.org/10.1016/j.urology.2011.09.031
Keeley, P. W., Foster, G., & Whitelaw, L. (2000). Hear my song: auditory hallucinations with tramadol hydrochloride. BMJ : British Medical Journal, 321(December 2000), 1608. https://doi.org/10.1136/bmj.321.7276.1608
Keskin, H. L., Keskin, E. A., Avsar, A. F., Tabuk, M., & Caglar, G. S. (2003). Pethidine versus tramadol for pain relief during labor. International Journal of Gynecology and Obstetrics, 82(1), 11–16. https://doi.org/10.1016/S0020-7292(03)00047-X
Khalifa, H. E., Darweesh, A., Hassaan, S., & Mostafa, S. (2018). Assessment of cognitive functions in tramadol-dependent patients. Middle East Current Psychiatry, 25(1), 2–5. https://doi.org/10.1097/01.XME.0000526928.54570
Khan, F., Yousef, H., & Errayes, M. (2010). Tramadol toxicity-induced rhabdomyolysis. Journal of Emergencies, Trauma, and Shock, 3(4), 421. https://doi.org/10.4103/0974-2700.70766
Khooshideh, M., & Shahriari, A. (2009). A comparison of tramadol and pethidine analgesia on the duration of labour: A randomised clinical trial. Australian and New Zealand Journal of Obstetrics and Gynaecology, 49(1), 59–63. https://doi.org/10.1111/j.1479-828X.2009.00949.x
Khosrojerdi, H., Talesh, G. A., Danaei, G. H., Saremi, S. S., Adab, A., & Afshari, R. (2015). Tramadol half life is dose dependent in overdose. DARU, Journal of Pharmaceutical Sciences, 23(1), 23–25. https://doi.org/10.1186/s40199-015-0104-y
Kirchheiner, J., Keulen, J. T. H. A., Bauer, S., Roots, I., & Brockmöller, J. (2008). Effects of the CYP2D6 gene duplication on the pharmacokinetics and pharmacodynamics of tramadol. Journal of Clinical Psychopharmacology, 28(1), 78–83. https://doi.org/10.1097/JCP.0b013e318160f827
Kitamura, A., Higuchi, K., Okura, T., & Deguchi, Y. (2014). Transport characteristics of tramadol in the blood-brain barrier. Journal of Pharmaceutical Sciences, 103(10), 3335–3341. https://doi.org/10.1002/jps.24129
Kitson, R., & Carr, B. (2005). Tramadol and severe serotonin syndrome. Anaesthesia, 60(9), 934–935. https://doi.org/10.1111/j.1365-2044.2005.04345.x
Knisely, J. S., Campbell, E. D., Dawson, K. S., & Schnoll, S. H. (2002). Tramadol post-marketing surveillance in health care professionals. Drug and Alcohol Dependence, 68(1), 15–22. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12167549
Kriikku, P. (n.d.). All the different ways to look at TRAMADOL DEATHS.
Künig, G., Dätwyler, S., Eschen, A., & Schreiter Gasser, U. (2006). Unrecognised Long-Lasting Tramadol-Induced Delirium in Two Elderly Patients: A Case Report. Pharmacopsychiatry, 39(5), 194–199. https://doi.org/10.1055/s-2006-948331
Kusari, S., Tatsimo, S. J. N., Zühlke, S., & Spiteller, M. (2016). Synthetic Origin of Tramadol in the Environment. Angewandte Chemie International Edition, 55(1), 240–243. https://doi.org/10.1002/anie.201508646
Kusari, S., Tatsimo, S. J. N., Zühlke, S., Talontsi, F. M., Kouam, S. F., & Spiteller, M. (2014). Tramadol – A True Natural Product. Angewandte Chemie – International Edition, 53(45), 12073–12076. https://doi.org/10.1002/anie.201406639
Lagard, C., Chevillard, L., Malissin, I., Ris�de, P., Callebert, J., Labat, L., … M�garbane, B. (2016). Mechanisms of tramadol-related neurotoxicity in the rat: Does diazepam/tramadol combination play a worsening role in overdose? Toxicology and Applied Pharmacology, 310, 108–119. https://doi.org/10.1016/j.taap.2016.09.013
Lagard, C., Malissin, I., Indja, W., Risède, P., Chevillard, L., & Mégarbane, B. (2018). Is naloxone the best antidote to reverse tramadol-induced neuro-respiratory toxicity in overdose? An experimental investigation in the rat. Clinical Toxicology, 56(8), 737–743. https://doi.org/10.1080/15563650.2017.1401080
Lakhal, M. H., Moula, O., Bahrini, L., Maamri, A., & Zalila, H. (2015). Psychosis Following Tramadol Withdrawal: a Case Report. European Psychiatry, 30, 1095. https://doi.org/10.1016/S0924-9338(15)30863-4
Lakhal, M. H., Moula, O., Maamri, A., & Zalila, H. (2015). Tramadol Dependence in a Tunisian Patient with No Previous Substance Misuse History. European Psychiatry, 30(0), 1098. https://doi.org/10.1016/S0924-9338(15)30866-X
Langley, P. C., Patkar, A. D., Boswell, K. A., Benson, C. J., & Schein, J. R. (2010). Adverse event profile of tramadol in recent clinical studies of chronic osteoarthritis pain. Current Medical Research and Opinion, 26(1), 239–251. https://doi.org/10.1185/03007990903426787
Lanier, R. K., Lofwall, M. R., Mintzer, M. Z., Bigelow, G. E., & Strain, E. C. (2010). Physical dependence potential of daily tramadol dosing in humans. Psychopharmacology, 211(4), 457–466. https://doi.org/10.1007/s00213-010-1919-3
Lassen, D., Damkier, P., & Brøsen, K. (2015). The Pharmacogenetics of Tramadol. Clinical Pharmacokinetics, 54(8), 825–836. https://doi.org/10.1007/s40262-015-0268-0
LAUGESEN, S., ENGGAARD, T., PEDERSEN, R., SINDRUP, S., & BROSEN, K. (2005). Paroxetine, a cytochrome P450 2D6 inhibitor, diminishes the stereoselective -demethylation and reduces the hypoalgesic effect of tramadol. Clinical Pharmacology & Therapeutics, 77(4), 312–323. https://doi.org/10.1016/j.clpt.2004.11.002
Lechowicz, W. (2000). Complex Intoxication by Tramadol and Tianeptine: a Case Report.
Lee, S. H., Cho, S. Y., Lee, H. G., Choi, J. I., Yoon, M. H., & Kim, W. M. (2013). Tramadol induced paradoxical hyperalgesia. Pain Physician, 16(1), 41–44.
Lee CR, McTavish D, S. E. (1993). Tramadol. A preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in acute and chronic pain states. Drugs, 46(2), 313–40.
Lehmann, K. A. (1994). Tramadol for the management of acute pain. Drugs, 47 Suppl 1, 19–32. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7517822
Lehmann, K. A., Gerhard, A., Horrichs‐Haermeyer, G., Grond, S., & Zech, D. (1991). Postoperative patient‐controlled analgesia with sufentanil: analgesic efficacy and minimum effective concentrations. Acta Anaesthesiologica Scandinavica. https://doi.org/10.1111/j.1399-6576.1991.tb03277.x
Leo, R. J., Narendran, R., & Deguiseppe, B. (2000). Methadone detoxification of tramadol dependence. Journal of Substance Abuse Treatment, 19(3), 297–299. https://doi.org/10.1016/S0740-5472(00)00098-2
Leppert, W., & Majkowicz, M. (2010). The impact of tramadol and dihydrocodeine treatment on quality of life of patients with cancer pain. International Journal of Clinical Practice, 64(12), 1681–1687. https://doi.org/10.1111/j.1742-1241.2010.02422.x
Lesani, A., Javadi-Paydar, M., Khodadad, T. K., Asghari-Roodsari, A., Shirkhodaei, M., Norouzi, A., & Dehpour, A. R. (2010). Involvement of the nitric oxide pathway in the anticonvulsant effect of tramadol on pentylenetetrazole-induced seizures in mice. Epilepsy and Behavior, 19(3), 290–295. https://doi.org/10.1016/j.yebeh.2010.08.006
Li, Q., Wang, R., Guo, Y., Wen, S., Xu, L., & Wang, S. (2010). Relationship of CYP2D6 genetic polymorphisms and the pharmacokinetics of tramadol in Chinese volunteers. Journal of Clinical Pharmacy and Therapeutics, 35(2), 239–247. https://doi.org/10.1111/j.1365-2710.2009.01102.x
Liu, Y. C., & Wang, W. S. (2012). Human mu-opioid receptor gene A118G polymorphism predicts the efficacy of tramadol/acetaminophen combination tablets (ultracet) in oxaliplatin-induced painful neuropathy. Cancer. https://doi.org/10.1002/cncr.26430
Loffredo, C. A., Boulos, D. N. K., Saleh, D. A., Jillson, I. A., Garas, M., Loza, N., … Amr, S. (2015). Substance Use by Egyptian Youth: Current Patterns and Potential Avenues for Prevention. Substance Use & Misuse, 50(5), 609–618. https://doi.org/10.3109/10826084.2014.997391
Lofwall, M. R., Walsh, S. L., Bigelow, G. E., & Strain, E. C. (2007). Modest opioid withdrawal suppression efficacy of oral tramadol in humans. Psychopharmacology, 194(3), 381–393. https://doi.org/10.1007/s00213-007-0847-3
Loram, L. C., Mitchell, D., Skosana, M., & Fick, L. G. (2007). Tramadol is more effective than morphine and amitriptyline against ischaemic pain but not thermal pain in rats. Pharmacological Research, 56(1), 80–85. https://doi.org/10.1016/j.phrs.2007.04.003
Loraschi, A., Galli, N., & Cosentino, M. (2014). Dietary supplement and drug use and doping knowledge and attitudes in italian young elite cyclists. Clinical Journal of Sport Medicine, 24(3), 238–244. https://doi.org/10.1097/JSM.0000000000000018
Lota, A. S., Dubrey, S. W., & Wills, P. (2012). Profound hyponatraemia following a tramadol overdose. QJM, 105(4), 397–398. https://doi.org/10.1093/qjmed/hcs027
Loughrey, M. B., Loughrey, C. M., Johnston, S., & O’Rourke, D. (2003). Fatal hepatic failure following accidental tramadol overdose. Forensic Science International, 134(2–3), 232–233. https://doi.org/10.1016/S0379-0738(03)00132-4
Lusthof, K. J., & Zweipfenning, P. G. (1998). Suicide by tramadol overdose. Journal of Analytical Toxicology, 22(3), 260. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9669891
Maclean, A. J. B., & Schwartz, T. L. (2015). Tramadol for the treatment of fibromyalgia. Expert Review of Neurotherapeutics, 15(5), 469–475. https://doi.org/10.1586/14737175.2015.1034693
Mannocchi, G., Napoleoni, F., Napoletano, S., Pantano, F., Santoni, M., Tittarelli, R., & Arbarello, P. (2013). Fatal self administration of tramadol and propofol: A case report. Journal of Forensic and Legal Medicine, 20(6), 715–719. https://doi.org/10.1016/j.jflm.2013.04.003
Manocha, A., Sharma, K. K., & Mediratta, P. K. (1998). Tramadol, a centrally acting opioid: Anticonvulsant effect against maximal electroshock seizure in mice. Indian Journal of Physiology and Pharmacology, 42(3), 407–411.
Manocha, A., Sharma, K. K., & Mediratta, P. K. (2005). On the mechanism of anticonvulsant effect of tramadol in mice. Pharmacology Biochemistry and Behavior, 82(1), 74–81. https://doi.org/10.1016/j.pbb.2005.07.013
Maréchal, C., Honorat, R., & Claudet, I. (2011). Serotonin Syndrome Induced by Tramadol Intoxication in an 8-Month-Old Infant. Pediatric Neurology, 44(1), 72–74. https://doi.org/10.1016/j.pediatrneurol.2010.08.005
Marquardt, K. A., Alsop, J. A., & Albertson, T. E. (2005). Tramadol Exposures Reported to Statewide Poison Control System. Annals of Pharmacotherapy, 39(6), 1039–1044. https://doi.org/10.1345/aph.1E577
Martinez, V., Guichard, L., & Fletcher, D. (2015). Effect of combining tramadol and morphine in adult surgical patients: A systematic review and meta-analysis of randomized trials. British Journal of Anaesthesia, 114(3), 384–395. https://doi.org/10.1093/bja/aeu414
Mason, B. J., & Blackburn, K. H. (1997). Possible serotonin syndrome associated with tramadol and sertraline coadministration. Annals of Pharmacotherapy, 31(2), 175–177. https://doi.org/10.1177/106002809703100208
Matouskova, O., Slanar, O., Chytil, L., & Perlik, F. (2011). Pupillometry in healthy volunteers as a biomarker of tramadol efficacy. Journal of Clinical Pharmacy and Therapeutics, 36(4), 513–517. https://doi.org/10.1111/j.1365-2710.2010.01203.x
Mattia, C., Mazzaferro, S., Coluzzi, F., & Luzi, M. (2004). Respiratory depression following iatrogenic tramadol overuse in a patient with chronic renal failure. The Journal of Headache and Pain, 5(2), 137–139. https://doi.org/10.1007/s10194-004-0076-7
Mayor, S. (2013). Drug experts call for stronger regulation of tramadol to reduce misuse. BMJ (Clinical Research Ed.), 346(February), 2013. https://doi.org/10.1136/bmj.f1264
McCarberg, B. (2007). Tramadol extended-release in the management of chronic pain. Therapeutics and Clinical Risk Management, 3(3), 401–10. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18488071
Mcdiarmid, T., & Mackler, L. (2005). What is the addiction risk associated with tramadol ? The Journal of Family Practice, 54(1), 5–7. Retrieved from http://www.jfponline.com/Pages.asp?AID=1849
Mehrpour, M. (2005). Intravenous Tramadol-Induced Seizure : Two Case Reports, 146–147.
Meymandi, M. S., & Keyhanfar, F. (2012). Pregabalin antinociception and its interaction with tramadol in acute model of pain. Pharmacological Reports, 64(3), 576–585. https://doi.org/10.1016/S1734-1140(12)70853-8
Michaud, K., Augsburger, M., Romain, N., Giroud, C., & Mangin, P. (1999). Fatal overdose of tramadol and alprazolam. Forensic Science International. https://doi.org/10.1016/S0379-0738(99)00118-8
Minami, K., Ogata, J., & Uezono, Y. (2015). What is the main mechanism of tramadol? Naunyn-Schmiedeberg’s Archives of Pharmacology, 388(10), 999–1007. https://doi.org/10.1007/s00210-015-1167-5
Minami, K., Sudo, Y., Miyano, K., Murphy, R. S., & Uezono, Y. (2015). µ-Opioid receptor activation by tramadol and O-desmethyltramadol (M1). Journal of Anesthesia, 29(3), 475–479. https://doi.org/10.1007/s00540-014-1946-z
Miotto, K., Cho, A. K., Khalil, M. A., Blanco, K., Sasaki, J. D., & Rawson, R. (2017). Trends in Tramadol: Pharmacology, Metabolism, and Misuse. Anesthesia and Analgesia, 124(1), 44–51. https://doi.org/10.1213/ANE.0000000000001683
Miranda, H. F., Noriega, V., Zepeda, R. J., Sierralta, F., & Prieto, J. C. (2012). Synergism Between Fentanyl and Tramadol in Tonic Inflammatory Pain: the Orofacial Formalin Test. Inflammation, 35(3), 1132–1137. https://doi.org/10.1007/s10753-011-9420-7
Miyano, K., Minami, K., Yokoyama, T., Ohbuchi, K., Yamaguchi, T., Murakami, S., … Uezono, Y. (2015). Tramadol and Its Metabolite M1 Selectively Suppress Transient Receptor Potential Ankyrin 1 Activity, but Not Transient Receptor Potential Vanilloid 1 Activity. Anesthesia and Analgesia, 120(4), 790–798. https://doi.org/10.1213/ANE.0000000000000625
Modi, H., Mazumdar, B., & Bhatt, J. (2013). Study of interaction of tramadol with amlodipine in mice. Indian Journal of Pharmacology, 45(1), 76. https://doi.org/10.4103/0253-7613.106440
Moore, A. R., & McQuay, J. H. (1997). Single-patient data meta-analysis of 3453 postoperative patients: oral tramadol versus placebo, codeine and combination analgesics. Pain, 69(3), 287–294. https://doi.org/10.1016/S0304-3959(96)03291-5
Moore, K. A., Cina, S. J., Jones, R., Selby, D. M., Levine, B., & Smith, M. L. (1999). Tissue distribution of tramadol and metabolites in an overdose fatality. The American Journal of Forensic Medicine and Pathology, 20(1), 98–100. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10208348
Moore, P. A., Crout, R. J., Jackson, D. L., Schneider, L. G., Graves, R. W., & Bakos, L. (1998). Tramadol hydrochloride: Analgesic efficacy compared with codeine, aspirin with codeine, and placebo after dental extraction. Journal of Clinical Pharmacology, 38(6), 554–560. https://doi.org/10.1002/j.1552-4604.1998.tb05794.x
Mugunthan, N., & Davoren, P. (2012). Danger of Hypoglycemia Due to Acute Tramadol Poisoning. Endocrine Practice, 18(6), e151–e152. https://doi.org/10.4158/EP12070.CR
Mukpo, A. (2017). How an improved understanding of drug use can contribute to peace and stability in Nigeria, (March), 1–6.
Mullican, W. S., Lacy, J. R., & TRAMAP-ANAG-006 Study Group. (2001). Tramadol/acetaminophen combination tablets and codeine/acetaminophen combination capsules for the management of chronic pain: a comparative trial. Clinical Therapeutics, 23(9), 1429–45. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11589258
Musshoff, F., & Madea, B. (2001). Fatality due to ingestion of tramadol alone. Forensic Science International, 116(2–3), 197–199. https://doi.org/10.1016/S0379-0738(00)00374-1
Nagakannan, P., Shivasharan, B. D., Thippeswamy, B. S., & Veerapur, V. P. (2012). Effect of tramadol on behavioral alterations and lipid peroxidation after transient forebrain ischemia in rats. Toxicology Mechanisms and Methods, 22(9), 674–678. https://doi.org/10.3109/15376516.2012.716092
Nair, S., & Chandy, T. (2015). Cardiac arrest from tramadol and fentanyl combination. Indian Journal of Anaesthesia, 59(4), 254. https://doi.org/10.4103/0019-5049.155008
Nasare, N. V., Banerjee, B. D., Suryakantrao Deshmukh, P., Mediratta, P. K., Saxena, A. K., Ahmed, R. S., & Bhattacharya, S. N. (2016). CYP2D6∗2 polymorphism as a predictor of failed outpatient tramadol therapy in postherpetic neuralgia patients. American Journal of Therapeutics, 23(3), e697–e707. https://doi.org/10.1097/MJT.0b013e31826fc491
Nasouhi, S., Talaie, H., Pajoumand, A., Aghapour, S., Rahimi, M., Khorasani, A. G., … Mahdavinejad, A. (2015). Hypo and hyperglycemia among tramadol overdose patients in Loghman Hakim Hospital, Tehran, Iran. Pakistan Journal of Pharmaceutical Sciences, 28(6), 1959–1963.
Nebhinani, N., Singh, S. M., & Gupta, G. (2013). A patient with Tramadol dependence and predictable provoked epileptic seizures. Indian J Psychiatry, 55(3), 293–294. https://doi.org/10.4103/0019-5545.117153
Nelson, E. M., & Philbrick, A. M. (2012). Evitando el síndrome de serotonina: La naturaleza de la interacción de drogas entre tramadol e inhibidores selectivos de recaptación de serotonina. Annals of Pharmacotherapy, 46(12), 1712–1716. https://doi.org/10.1345/aph.1Q748
Nelson, L. S., & Juurlink, D. N. (2015). Tramadol and hypoglycemia one more thing toworry about. JAMA Internal Medicine, 175(2), 194–195. https://doi.org/10.1001/jamainternmed.2014.5260
Norrbrink, C., & Lundeberg, T. (2009). Tramadol in Neuropathic Pain After Spinal Cord Injury. The Clinical Journal of Pain, 25(3), 177–184. https://doi.org/10.1097/AJP.0b013e31818a744d
O’Connor, E. C., & Mead, A. N. (2010). Tramadol acts as a weak reinforcer in the rat self-administration model, consistent with its low abuse liability in humans. Pharmacology Biochemistry and Behavior, 96(3), 279–286. https://doi.org/10.1016/j.pbb.2010.05.018
Ogata, J., Minami, K., Uezono, Y., Okamoto, T., Shiraishi, M., Shigematsu, A., & Ueta, Y. (2004). The Inhibitory Effects of Tramadol on 5-Hydroxytryptamine Type 2C Receptors Expressed in Xenopus Oocytes. Anesthesia & Analgesia, 98(5), 1401–1406. https://doi.org/10.1213/01.ANE.0000108963.77623.A4
Ogawa, K., Tateno, A., Arakawa, R., Sakayori, T., Ikeda, Y., Suzuki, H., & Okubo, Y. (2014). Occupancy of serotonin transporter by tramadol: A positron emission tomography study with [11C]DASB. International Journal of Neuropsychopharmacology, 17(6), 845–850. https://doi.org/10.1017/S1461145713001764
Olsson, M. O., Öjehagen, A., Brådvik, L., Kronstrand, R., & Håkansson, A. (2017). High Rates of Tramadol Use among Treatment-Seeking Adolescents in Malmö, Sweden: A Study of Hair Analysis of Nonmedical Prescription Opioid Use. Journal of Addiction, 2017, 6716929. https://doi.org/10.1155/2017/6716929
Orbach-Zinger, S., Paul-Keslin, L., Nichinson, E., Chinchuck, A., Nitke, S., & Eidelman, L. A. (2012). Tramadol-metoclopramide or remifentanil for patient-controlled analgesia during second trimester abortion: A double-blinded, randomized controlled trial. Journal of Clinical Anesthesia, 24(1), 28–32. https://doi.org/10.1016/j.jclinane.2011.05.003
Orliaguet, G., Hamza, J., Couloigner, V., Denoyelle, F., Loriot, M.-A., Broly, F., & Garabedian, E. N. (2015). A Case of Respiratory Depression in a Child With Ultrarapid CYP2D6 Metabolism After Tramadol. Pediatrics, 135(3), e753–e755. https://doi.org/10.1542/peds.2014-2673
Özer, Z., Görür, K., Altunkan, A. A., Bilgin, E., Çamdeviren, H., & Oral, U. (2003). Efficacy of tramadol versus meperidine for pain relief and safe recovery after adenotonsillectomy. European Journal of Anaesthesiology. https://doi.org/10.1017/S0265021503001480
Panksepp, J. (2017). Use of tramadol in psychiatric care: A comprehensive review and report of two cases. Swiss Medical Weekly, 147(1920). https://doi.org/10.4414/smw.2017.14428
Park, S. H., Wackernah, R. C., & Stimmel, G. L. (2014). Serotonin syndrome: is it a reason to avoid the use of tramadol with antidepressants? Journal of Pharmacy Practice, 27(1), 71–8. https://doi.org/10.1177/0897190013504957
Peacock, L. E., & Wright, F. (2011). Serotonin syndrome secondary to tramadol and citalopram. Age and Ageing, 40(4), 528–528. https://doi.org/10.1093/ageing/afr017
Pellegrino, P., Carnovale, C., Borsadoli, C., Danini, T., Speziali, A., Perrone, V., … Radice, S. (2013). Two cases of hallucination in elderly patients due to a probable interaction between flu immunization and tramadol. European Journal of Clinical Pharmacology, 69(8), 1615–1616. https://doi.org/10.1007/s00228-013-1517-5
Perdreau, E., Iriart, X., Mouton, J. B., Jalal, Z., & Thambo, J. B. (2015). Cardiogenic shock due to acute tramadol intoxication. Cardiovascular Toxicology, 15(1), 100–103. https://doi.org/10.1007/s12012-014-9262-2
Petramfar, P., & Borhani Haghighi, A. (2010). Tramadol induced seizure: Report of 106 patients. Iranian Red Crescent Medical Journal, 12(1), 49–51. Retrieved from http://www.scopus.com/inward/record.url?eid=2-s2.0-73849119644&partnerID=tZOtx3y1
Pollice, R., Casacchia, M., Bianchini, V., Mazza, M., Conti, C. M., & Roncone, R. (2008). Severe tramadol addiction in a 61 year-old woman without a history of substance abuse. International Journal of Immunopathology and Pharmacology, 21(2), 475–476.
Pothiawala, S., & Ponampalam, R. (2011). Tramadol overdose: A case report. Proceedings of Singapore Healthcare, 20(3), 219–223. https://doi.org/10.1177/201010581102000311
Potschka, H., Friderichs, E., & Löscher, W. (2000). Anticonvulsant and proconvulsant effects of tramadol, its enantiomers and its M1 metabolite in the rat kindling model of epilepsy. British Journal of Pharmacology, 131(2), 203–212. https://doi.org/10.1038/sj.bjp.0703562
Poulsen, L., Arendt-Nielsen, L., Brøsen, K., & Sindrup, S. H. (1996). The hypoalgesic effect of tramadol in relation to CYP2D6*. Clinical Pharmacology & Therapeutics, 60(6), 636–644. https://doi.org/10.1016/S0009-9236(96)90211-8
Pradeep Kumar, K., Kumar Kulkarni, D., Indira, & Gopinath. (2013). Pregabalin versus tramadol for postoperative pain management in patients undergoing lumbar laminectomy: a randomized, double-blinded, placebo-controlled study. Journal of Pain Research, 471. https://doi.org/10.2147/JPR.S43613
Preston KL, Jasinski DR, T. M. (1991). Abuse potential and pharma- cological comparison of tramadol and morphine. Drug Alcohol Depend, 27(1), 7–17.
Progler, Y. (2010). Drug addiction in Gaza and the illicit trafficking of Tramadol. Journal of Research in Medical Sciences, 15(3), 185–188.
Radbruch, L., Glaeske, G., Grond, S., Münchberg, F., Scherbaum, N., Storz, E., … Cremer-Schaeffer, P. (2013). Topical Review on the Abuse and Misuse Potential of Tramadol and Tilidine in Germany. Substance Abuse, 34(3), 313–320. https://doi.org/10.1080/08897077.2012.735216
Raffa, R. B., Friderichs, E., Reimann, W., Shank, R. P., Codd, E. E., Vaught, J. L., … Selve, N. (1992). Complementary andSynergistic Antinociceptive Interaction betweenthe Enantiomers of Tramadol. J Pharmacol Exp Ther., 267(1), 331–40.
Rahimi, H. R., Soltaninejad, K., & Shadnia, S. (2014). Acute tramadol poisoning and its clinical and laboratory findings. Journal of Research in Medical Sciences, 19(9), 855–859.
Rahimi, S. Y., Alleyne, C. H., Vernier, E., Witcher, M. R., & Vender, J. R. (2010). Postoperative pain management with tramadol after craniotomy: evaluation and cost analysis. Journal of Neurosurgery, 112(2), 268–272. https://doi.org/10.3171/2008.9.17689
Raiger, L., Naithani, U., Bhatia, S., & Chauhan, S. (2012). Seizures after intravenous tramadol given as premedication. Indian Journal of Anaesthesia, 56(1), 55. https://doi.org/10.4103/0019-5049.93345
Rajabizadeh, G., Kheradmand, A., & Nasirian, M. (2009). Psychosis following Tramadol Withdrawal. Addiction & Health, 1(1), 58–61. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24494084
Randall, C., & Crane, J. (2014). Tramadol deaths in Northern Ireland: A review of cases from 1996 to 2012. Journal of Forensic and Legal Medicine, 23, 32–36. https://doi.org/10.1016/j.jflm.2014.01.006
Reeves, R. R., & Cox, S. K. (2008). Similar effects of tramadol and venlafaxine in major depressive disorder. Southern Medical Journal, 101(2), 193–5. https://doi.org/10.1097/SMJ.0b013e3181616e66
Rehni, A. K., Singh, I., & Kumar, M. (2008). Tramadol-induced seizurogenic effect: A possible role of opioid-dependent ??-aminobutyric acid inhibitory pathway. Basic and Clinical Pharmacology and Toxicology. https://doi.org/10.1111/j.1742-7843.2008.00276.x
Rehni, A. K., Singh, T. G., Singh, N., & Arora, S. (2010). Tramadol-induced seizurogenic effect: A possible role of opioid-dependent histamine (H1) receptor activation-linked mechanism. Naunyn-Schmiedeberg’s Archives of Pharmacology, 381(1), 11–19. https://doi.org/10.1007/s00210-009-0476-y
Reig, E. (2002). Tramadol in musculoskeletal pin – A survey. Clinical Rheumatology, 21(1 SUPPL.), S9–S12. Retrieved from http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L34248142%5Cnhttp://va8ef7lf8s.search.serialssolutions.com/?sid=EMBASE&issn=07703198&id=doi:&atitle=Tramadol+in+musculoskeletal+pin+-+A+survey&stitle=Clin.+Rheumatol.&title=Clinical+Rhe
Reimann, W., & Schneider, F. (1998). Induction of 5-hydroxytryptamine release by tramadol, fenfluramine and reserpine. European Journal of Pharmacology, 349(2–3), 199–203. https://doi.org/10.1016/S0014-2999(98)00195-2
Riedel, F., & v. Stockhausen, H. B. (1984). Severe cerebral depression after intoxication with tramadol in a 6-month-old infant. European Journal of Clinical Pharmacology, 26(5), 631–632. https://doi.org/10.1007/BF00543498
Ripamonti, C., Fagnoni, E., & De Conno, F. (2004). Withdrawal syndrome after delayed tramadol intake. American Journal of Psychiatry, 161(12), 2326–2327. https://doi.org/10.1176/appi.ajp.161.12.2326
Rodieux, F., Vutskits, L., Posfay-Barbe, K. M., Habre, W., Piguet, V., Desmeules, J. A., & Samer, C. F. (2018). When the safe alternative is not that safe: Tramadol prescribing in children. Frontiers in Pharmacology, 9(MAR), 1–13. https://doi.org/10.3389/fphar.2018.00148
Rodriguez Villamañan, J. C., Albaladejo Blanco, C., Sanchez Sanchez, A., Carvajal, A., Martin Arias, L., & Garcia del Pozo, J. (2000). Withdrawal syndrome after long-term treatment with tramadol. The British Journal of General Practice : The Journal of the Royal College of General Practitioners, 50(454), 406. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10897546
Rojas-Corrales, M. O., Berrocoso, E., Gibert-Rahola, J., & Micó, J. A. (2002). Antidepressant-like effects of tramadol and other central analgesics with activity on monoamines reuptake, in helpless rats. Life Sciences, 72(2), 143–152. https://doi.org/10.1016/S0024-3205(02)02220-8
Rojas-Corrales, M. O., Gibert-Rahola, J., & Micó, J. A. (1998). Tramadol induces antidepressant-type effects in mice. Life Sciences, 63(12), 175–180. https://doi.org/10.1016/S0024-3205(98)00369-5
Rothman, R., & Baumann, M. (2006). Therapeutic Potential of Monoamine Transporter Substrates. Current Topics in Medicinal Chemistry, 6(17), 1845–1859. https://doi.org/10.2174/156802606778249766
Ryan, N. M., & Isbister, G. K. (2015). Tramadol overdose causes seizures and respiratory depression but serotonin toxicity appears unlikely. Clinical Toxicology, 53(6), 545–550. https://doi.org/10.3109/15563650.2015.1036279
Sacerdote, P., Bianchi, M., Gaspani, L., Manfredi, B., Maucione, A., Terno, G., … Panerai, A. E. (2000). The Effects of Tramadol and Morphine on Immune Responses and Pain After Surgery in Cancer Patients. Anesthesia & Analgesia, 90(6), 1411–1414. https://doi.org/10.1097/00000539-200006000-00028
Sachdeva, D. K., & Jolly, B. T. (1997). Tramadol overdose requiring prolonged opioid antagonism. The American Journal of Emergency Medicine, 15(2), 217–8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9115538
Salm-Reifferscheidt, L. (2018). Tramadol: Africa’s opioid crisis. The Lancet, 391(10134), 1982–1983. https://doi.org/10.1016/S0140-6736(18)31073-0
Sansone, R. A., & Sansone, L. A. (2009). Tramadol: seizures, serotonin syndrome, and coadministered antidepressants. Psychiatry (Edgmont (Pa. : Township)), 6(4), 17–21. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19724727
Santacroce, R., Bosio, E., Scioneri, V., & Mignone, M. (2018). The new drugs and the sea: The phenomenon of narco-terrorism. International Journal of Drug Policy, 51, 67–68. https://doi.org/10.1016/j.drugpo.2017.10.012
Santos Garcia, J. B., Lech, O., Campos Kraychete, D., Rico, M. A., Hernández-Castro, J. J., Colimon, F., … Bonilla Sierra, P. (2017). The role of tramadol in pain management in Latin America: a report by the Change Pain Latin America Advisory Panel. Current Medical Research and Opinion, 33(9), 1615–1621. https://doi.org/10.1080/03007995.2017.1354821
Sarkar, S., Nebhinani, N., Singh, S., Mattoo, S., & Basu, D. (2012). Tramadol dependence: A case series from India. Indian Journal of Psychological Medicine, 34(3), 283. https://doi.org/10.4103/0253-7176.106038
Sawynok, J., Reid, A. R., & Liu, J. (2013). Spinal and peripheral adenosine A1 receptors contribute to antinociception by tramadol in the formalin test in mice. European Journal of Pharmacology, 714(1–3), 373–378. https://doi.org/10.1016/j.ejphar.2013.07.012
Schnabel, A., Reichl, S. U., Meyer-Frießem, C., Zahn, P. K., & Pogatzki-Zahn, E. (2015). Tramadol for postoperative pain treatment in children. Cochrane Database of Systematic Reviews, (3), 1–73. https://doi.org/10.1002/14651858.CD009574.pub2
Schug, S. A. (2007). The role of tramadol in current treatment strategies for musculoskeletal pain. Therapeutics and Clinical Risk Management, 3(5), 717–23. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18472996
Science, T. (2015). Tramadol Dependency Treatment: A New Approach. Journal of Addiction Medicine and Therapeutic Science, 1(2), 041–043. https://doi.org/10.17352/2455-3484.000010
Senay, E. C., Adams, E. H., Geller, A., Inciardi, J. A., Munoz, A., Schnoll, S. H., … Cicero, T. J. (2003). Physical dependence on Ultram((R)) (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend, 69(3), 233–241. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12633909
Sevimli, Z. U., Dursun, H., & Erdogan, F. (2006). Histopathologic changes in liver induced by morphine and tramadol. The Pain Clinic, 18(4), 321–325. https://doi.org/10.1163/156856906778704687
Shadnia, S., Brent, J., Mousavi-Fatemi, K., Hafezi, P., & Soltaninejad, K. (2012). Recurrent Seizures in Tramadol Intoxication: Implications for Therapy Based on 100 Patients. Basic & Clinical Pharmacology & Toxicology, 111(2), n/a-n/a. https://doi.org/10.1111/j.1742-7843.2012.00874.x
Shadnia, S., Soltaninejad, K., Heydari, K., Sasanian, G., & Abdollahi, M. (2008). Tramadol intoxication: A review of 114 cases. Human and Experimental Toxicology, 27(3), 201–205. https://doi.org/10.1177/0960327108090270
Shahani, L. (2012). Tramadol Precipitating Serotonin Syndrome in a Patient on Antidepressants. The Journal of Neuropsychiatry and Clinical Neurosciences, 24(4), E52–E52. https://doi.org/10.1176/appi.neuropsych.11110343
Shapira, N. A., Keck, P. E., Goldsmith, T. D., McConville, B. J., Eis, M., & McElroy, S. L. (1997). Open-label pilot study of tramadol hydrochloride in treatment-refractory obsessive-compulsive disorder. Depression and Anxiety. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9559288
Sheikholeslami, B., Hamidi, M., Lavasani, H., Sharifzadeh, M., & Rouini, M. R. (2012). Lack of evidence for involvement of P-glycoprotein in brain uptake of the centrally acting analgesic, tramadol in the rat. Journal of Pharmacy and Pharmaceutical Sciences, 15(5), 606–615.
Shen, X. F., Wang, F. Z., Xu, S. Q., Ma, L., Liu, Y. S., Feng, S. W., … Guan, X. N. (2008). Comparison of the analgesic efficacy of preemptive and preventive tramadol after lumpectomy. Pharmacological Reports, 60(3), 415–421.
Siddik-Sayyid, S., Aouad-Maroun, M., Sleiman, D., Sfeir, M., & Baraka, A. (1999). Epidural tramadol for postoperative pain after Cesarean section. Canadian Journal of Anaesthesia, 46(8), 731–735. https://doi.org/10.1007/BF03013907
Sindrup, S. H., Andersen, G., Madsen, C., Smith, T., Brøsen, K., & Jensen, T. S. (1999). Tramadol relieves pain and allodynia in polyneuropathy: A randomised, double-blind, controlled trial. Pain, 83(1), 85–90. https://doi.org/10.1016/S0304-3959(99)00079-2
Sobey, P. W., Parran, T. V., Grey, S. F., Adelman, C. L., & Yu, J. (2004). The Use of Tramadol for Acute Heroin Withdrawal. Journal of Addictive Diseases, 22(4), 13–25. https://doi.org/10.1300/J069v22n04_03
Sousa, A. M., & Ashmawi, H. A. (2015). Local analgesic effect of tramadol is not mediated by opioid receptors in early postoperative pain in rats. Brazilian Journal of Anesthesiology (Elsevier), 65(3), 186–190. https://doi.org/10.1016/j.bjane.2014.06.006
Spencer, C. (2000). The Efficacy of Intramuscular Tramadol as a Rapid-Onset Antidepressant. Australian and New Zealand Journal of Psychiatry, 34(6), 1032–1033. https://doi.org/10.1177/000486740003400101
Spies, P. E., Willems, R., Pot, H., Bos, J. M., & Kramers, C. (2015). Interaction between Tramadol and SSRI’s: do we care? Clinical Therapeutics, 37(8), e43. https://doi.org/10.1016/j.clinthera.2015.05.130
Spiller, H. A., Gorman, S. E., Villalobos, D., Benson, B. E., Ruskosky, D. R., Stancavage, M. M., & Anderson, D. L. (1997). Prospective Multicenter Evaluation of Tramadol Exposure. Journal of Toxicology: Clinical Toxicology, 35(4), 361–364. https://doi.org/10.3109/15563659709043367
Stamer, U. M., Lehnen, K., Höthker, F., Bayerer, B., Wolf, S., Hoeft, A., & Stuber, F. (2003). Impact of CYP2D6 genotype on postoperative tramadol analgesia. Pain, 105(1–2), 231–238. https://doi.org/10.1016/S0304-3959(03)00212-4
Stamer, U. M., Musshoff, F., Kobilay, M., Madea, B., Hoeft, A., & Stuber, F. (2007). Concentrations of tramadol and O-desmethyltramadol enantiomers in different CYP2D6 genotypes. Clinical Pharmacology and Therapeutics. https://doi.org/10.1038/sj.clpt.6100152
Stamer, U. M., Musshoff, F., Stüber, F., Brockmöller, J., Steffens, M., & Tzvetkov, M. V. (2016). Loss-of-function polymorphisms in the organic cation transporter OCT1 are associated with reduced postoperative tramadol consumption. Pain, 157(11), 2467–2475. https://doi.org/10.1097/j.pain.0000000000000662
Stamer, U. M., Stüber, F., Muders, T., & Musshoff, F. (2008). Respiratory Depression with Tramadol in a Patient with Renal Impairment and CYP2D6 Gene Duplication. Anesthesia & Analgesia, 107(3), 926–929. https://doi.org/10.1213/ane.0b013e31817b796e
Stassinos, G. L., Gonzales, L., & Klein-Schwartz, W. (2017). Characterizing the Toxicity and Dose-Effect Profile of Tramadol Ingestions in Children. Pediatric Emergency Care, 0(0), 1–4. https://doi.org/10.1097/PEC.0000000000001084
Stoops, W. W., Lofwall, M. R., Nuzzo, P. A., Craig, L. B., Siegel, A. J., & Walsh, S. L. (2012). Pharmacodynamic profile of tramadol in humans: Influence of naltrexone pretreatment. Psychopharmacology, 223(4), 427–438. https://doi.org/10.1007/s00213-012-2739-4
Sudheer, P. S., Logan, S. W., Terblanche, C., Ateleanu, B., & Hall, J. E. (2007). Comparison of the analgesic efficacy and respiratory effects of morphine, tramadol and codeine after craniotomy. Anaesthesia, 62(6), 555–560. https://doi.org/10.1111/j.1365-2044.2007.05038.x
Sun, H. L., Zheng, J. W., Wang, K., Liu, R. K., & Liang, J. H. (2003). Tramadol reduces the 5-HTP-induced head-twitch response in mice via the activation of μ and κ opioid receptors. Life Sciences. https://doi.org/10.1016/S0024-3205(02)02345-7
Taghaddosinejad, F., Mehrpour, O., Afshari, R., Seghatoleslami, A., Abdollahi, M., & Dart, R. C. (2011). Factors Related to Seizure in Tramadol Poisoning and Its Blood Concentration. Journal of Medical Toxicology, 7(3), 183–188. https://doi.org/10.1007/s13181-011-0168-0
Tajes Alonso, M., Ramos Rios, R., Lopez Moriñigo, J. D., Espiño Diaz, I., Perez Garcia, M., Varela Casal, P., … Páramo Fernández, M. (2007). Musical hallucinations induced by tramadol. European Psychiatry, 22(2007), S336. https://doi.org/10.1016/j.eurpsy.2007.01.1145
Takhtfooladi, H. A., Takhtfooladi, M. A., Karimi, P., Asl, H. A., & Mousavi Nasab Mobarakeh, S. Z. (2014). Influence of tramadol on ischemia-reperfusion injury of rats’ skeletal muscle. International Journal of Surgery, 12(9), 963–968. https://doi.org/10.1016/j.ijsu.2014.07.015
Takhtfooladi, M. A., Jahanshahi, A., Sotoudeh, A., Daneshi, M. H., Aslani, K., & Takhtfooladi, H. A. (2014). Neuroprotective effects of tramadol on cerebral injuries caused by hind limb ischaemia/reperfusion in rats. Comparative Clinical Pathology, 23(5), 1141–1146. https://doi.org/10.1007/s00580-013-1753-1
Talaie, H., Panahandeh, R., Fayaznouri, M. R., Asadi, Z., & Abdollahi, M. (2009). Dose-independent occurrence of seizure with tramadol. Journal of Medical Toxicology, 5(2), 63–67. https://doi.org/10.1007/BF03161089
Tanne, C., Javouhey, E., Millet, A., & Bordet, F. (2016). Severe Tramadol Overdoses in Children: A Case Series Admitted to Paediatric Intensive Care Unit. Journal of Clinical Toxicology, 6(5), 1–5. https://doi.org/10.4172/2161-0495.1000317
Tantry, T., Shetty, P., Kadam, D., & Adappa, K. (2011). Tramadol-induced respiratory depression in a morbidly obese patient with normal renal function. Indian Journal of Anaesthesia, 55(3), 318. https://doi.org/10.4103/0019-5049.82667
Tarkkila, P., Tuominen, M., & Lindgren, L. (1998). Comparison of respiratory effects of tramadol and pethidine. European Journal of Anaesthesiology, 15(1), 64–68. https://doi.org/10.1046/j.1365-2346.1998.0233a.x
Tashakori, A., & Afshari, R. (2010). Tramadol overdose as a cause of serotonin syndrome: A case series. Clinical Toxicology, 48(4), 337–341. https://doi.org/10.3109/15563651003709427
Tetsunaga, T., Tetsunaga, T., Tanaka, M., & Ozaki, T. (2015). Efficacy of tramadol–acetaminophen tablets in low back pain patients with depression. Journal of Orthopaedic Science, 20(2), 281–286. https://doi.org/10.1007/s00776-014-0674-4
Thévenin, A., Beloeil, H., Blanie, A., Benhamou, D., & Mazoit, J.-X. (2008). The Limited Efficacy of Tramadol in Postoperative Patients: A Study of ED80 Using the Continual Reassessment Method. Anesthesia & Analgesia, 106(2), 622–627. https://doi.org/10.1213/ane.0b013e31816053aa
Thorn, D. A., Zhang, Y., Peng, B.-W., Winter, J. C., & Li, J.-X. (2011). Effects of imidazoline I2 receptor ligands on morphine- and tramadol-induced antinociception in rats. European Journal of Pharmacology, 670(2–3), 435–440. https://doi.org/10.1016/j.ejphar.2011.09.173
Tjäderborn, M., Jönsson, A. K., Ahlner, J., & Hägg, S. (2009). Tramadol dependence: a survey of spontaneously reported cases in Sweden. Pharmacoepidemiology and Drug Safety, 18(12), 1192–1198. https://doi.org/10.1002/pds.1838
Tjäderborn, M., Jönsson, A. K., Hägg, S., & Ahlner, J. (2007). Fatal unintentional intoxications with tramadol during 1995-2005. Forensic Science International, 173(2–3), 107–111. https://doi.org/10.1016/j.forsciint.2007.02.007
Tzvetkov, M. V., Saadatmand, A. R., Lötsch, J., Tegeder, I., Stingl, J. C., & Brockmöller, J. (2011). Genetically polymorphic OCT1: Another piece in the puzzle of the variable pharmacokinetics and pharmacodynamics of the opioidergic drug tramadol. Clinical Pharmacology and Therapeutics, 90(1), 143–150. https://doi.org/10.1038/clpt.2011.56
Ubale, V., Jaju, J., Gosavi, P., Pawar, G., Dharmadhikari, S., & Parekar, S. (2015). Evaluation of antidepressant activity of tramadol in mice: an experimental study. International Journal of Basic and Clinical Pharmacology, 4(3), 463–468. https://doi.org/10.18203/2319-2003.ijbcp20150017
Uysal, H. Y., Takmaz, S. A., Yaman, F., Baltaci, B., & Başar, H. (2011). The efficacy of intravenous paracetamol versus tramadol for postoperative analgesia after adenotonsillectomy in children. Journal of Clinical Anesthesia, 23(1), 53–57. https://doi.org/10.1016/j.jclinane.2010.07.001
VICKERS, M. D., O’FLAHERTY, D., SZEKELY, S. M., READ, M., & YOSHIZUMI, J. (1992). Tramadol: pain relief by an opioid without depression of respiration. Anaesthesia, 47(4), 291–296. https://doi.org/10.1111/j.1365-2044.1992.tb02166.x
Viegas, O. A. C., Khaw, B., & Ratnam, S. S. (1993). Tramadol in labour pain in primiparous patients. A prospective comparative clinical trial. European Journal of Obstetrics and Gynecology and Reproductive Biology, 49(3), 131–135. https://doi.org/10.1016/0028-2243(93)90260-J
Volpe, D. A., Tobin, G. A. M. M., Mellon, R. D., Katki, A. G., Parker, R. J., Colatsky, T., … Verbois, S. L. (2011). Uniform assessment and ranking of opioid Mu receptor binding constants for selected opioid drugs. Regulatory Toxicology and Pharmacology, 59(3), 385–390. https://doi.org/10.1016/j.yrtph.2010.12.007
Wagner, R., Piler, P., Bedanova, H., Adamek, P., Grodecka, L., & Freiberger, T. (2010). Myocardial injury is decreased by late remote ischaemic preconditioning and aggravated by tramadol in patients undergoing cardiac surgery: a randomised controlled trial☆. Interactive CardioVascular and Thoracic Surgery, 11(6), 758–762. https://doi.org/10.1510/icvts.2010.243600
Wang, S.-Q., Li, C.-S., & Song, Y.-G. (2009). Multiply organ dysfunction syndrome due to tramadol intoxication alone. The American Journal of Emergency Medicine, 27(7), 903.e5-903.e7. https://doi.org/10.1016/j.ajem.2008.11.013
Wentland, M. P., Lou, R., Lu, Q., Bu, Y., VanAlstine, M. A., Cohen, D. J., & Bidlack, J. M. (2009). Syntheses and opioid receptor binding properties of carboxamido-substituted opioids. Bioorganic & Medicinal Chemistry Letters, 19(1), 203–208. https://doi.org/10.1016/j.bmcl.2008.10.134
White, M., Division, T., & Health, P. (n.d.). Tramadol deaths in the United Kingdom. Public Health England.
WHO. (2014). Tramadol.
Wiffen, P. J., Derry, S., & Moore, R. A. (2017). Tramadol with or without paracetamol (acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews, (5), 10–13. https://doi.org/10.1002/14651858.CD012508.pub2
Wilder-Smith, C. H., Hill, L., Spargo, K., & Kalla, A. (2001). Treatment of severe pain from osteoarthritis with slow-release tramadol or dihydrocodeine in combination with NSAID’s: A randomised study comparing analgesia, antinociception and gastrointestinal effects. Pain, 91(1–2), 23–31. https://doi.org/10.1016/S0304-3959(00)00414-0
Winstock, A., Bell, J., & Borschmann, R. (2013). Friends, doctors, and tramadol: We might have a problem. BMJ (Online), 347(7925), 5599. https://doi.org/10.1136/bmj.f5599
Winstock, A. R., Borschmann, R., & Bell, J. (2014). The non-medical use of tramadol in the UK: findings from a large community sample. International Journal of Clinical Practice, 68(9), 1147–1151. https://doi.org/10.1111/ijcp.12429
Wolfe, F. (2000). Is tramadol “effective” in fibromyalgia? Implications for study design and clinical effectiveness. Jcr-Journal of Clinical Rheumatology. Retrieved from isi:000089828800001
Xia, M., Tong, J.-H., Zhou, Z.-Q., Duan, M.-L., Xu, J.-G., Zeng, H.-J., & Wang, S.-H. (2016). Tramadol inhibits proliferation, migration and invasion via α2-adrenoceptor signaling in breast cancer cells. European Review for Medical and Pharmacological Sciences, 20(1), 157–65. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26813469
Xu, J., Zhang, X. C., Lv, X. Q., Xu, Y. Y., Wang, G. X., Jiang, B., … Cai, X. J. (2014). Effect of the cytochrome P450 2D6*10 genotype on the pharmacokinetics of tramadol in post-operative patients. Pharmazie, 69(2), 138–141. https://doi.org/10.1691/ph.2014.3749
Yalcin, I., Aksu, F., Bodard, S., Chalon, S., & Belzung, C. (2007). Antidepressant-like effect of tramadol in the unpredictable chronic mild stress procedure: Possible involvement of the noradrenergic system. Behavioural Pharmacology, 18(7), 623–631. https://doi.org/10.1097/FBP.0b013e3282eff109
Yalcin, I., Coubard, S., Bodard, S., Chalon, S., & Belzung, C. (2008). Effects of 5,7-dihydroxytryptamine lesion of the dorsal raphe nucleus on the antidepressant-like action of tramadol in the unpredictable chronic mild stress in mice. Psychopharmacology, 200(4), 497–507. https://doi.org/10.1007/s00213-008-1227-3
Yanarates, O., Dogrul, A., Yildirim, V., Sahin, A., Sizlan, A., Seyrek, M., … Aypar, U. (2010). Spinal 5-HT7 Receptors Play an Important Role in the Antinociceptive and Antihyperalgesic Effects of Tramadol and Its Metabolite, O-Desmethyltramadol, via Activation of Descending Serotonergic Pathways. Anesthesiology, 112(3), 696–710. https://doi.org/10.1097/ALN.0b013e3181cd7920
Yang, C., Li, X., Wang, N., Xu, S., Yang, J., & Zhou, Z. (2012). Tramadol reinforces antidepressant effects of ketamine with increased levels of brain-derived neurotrophic factor and tropomyosin-related kinase B in rat hippocampus. Frontiers of Medicine in China, 6(4), 411–415. https://doi.org/10.1007/s11684-012-0226-2
Yarkan Uysal, H., Bilimgut, B., Dikmen, B., Inan, N., Ülger, G., & Eruyar, S. (2011). Epileptic Seizure Following IV Tramadol in a Patient with Mental Retardation and Cerebellar Ataxia. Pain Medicine, 12(5), 833–836. https://doi.org/10.1111/j.1526-4637.2011.01079.x
Yates, W. R., Nguyen, M. H., & Warnock, J. K. (2001). Tramadol dependence with no history of substance abuse. American Journal of Psychiatry. https://doi.org/10.1176/appi.ajp.158.6.964
Yoshizawa, K., Kawai, K., Fujie, M., Suzuki, J., Ogawa, Y., Yajima, T., & Yokomori, J. (2015). Overall safety profile and effectiveness of tramadol hydrochloride/acetaminophen in patients with chronic noncancer pain in Japanese real-world practice. Current Medical Research and Opinion, 31(11), 2119–2129. https://doi.org/10.1185/03007995.2015.1091975
Young, J. W. S., & Juurlink, D. N. (2013). Tramadol. Canadian Medical Association Journal, 185(8), E352–E352. https://doi.org/10.1503/cmaj.121592
Zarghami, M., Masoum, B., & Shiran, M.-R. (2012). Tramadol versus Methadone for Treatment of Opiate Withdrawal: A Double-Blind, Randomized, Clinical Trial. Journal of Addictive Diseases, 31(2), 112–117. https://doi.org/10.1080/10550887.2012.665728
Zhang, L.-Z., & Guo, Z. (2009). Tramadol reduces myocardial infarct size and expression and activation of nuclear factor kappa B in acute myocardial infarction in rats. European Journal of Anaesthesiology, 26(12), 1048–1055. https://doi.org/10.1097/EJA.0b013e32832c785d
Zhang, M., Jing, L., Liu, Q., Wen, R. T., Li, J. X., Li, Y. L., … Liang, J. H. (2012). Tramadol induces conditioned place preference in rats: Interactions with morphine and buprenorphine. Neuroscience Letters, 520(1), 87–91. https://doi.org/10.1016/j.neulet.2012.05.037