3-Methoxyphencyclidine (3-MeO-PCP) is an analog of the dissociative anesthetic phencyclidine (PCP). Although it first appeared in the scientific literature in the late 1970s and human use was discussed beginning in the late 1990s, it only became a widely used novel psychoactive substance (NPS) in the 2010s.
The drug produces dose-dependent disconnection from one’s body and surroundings, while also altering mood, anxiety, perception, and thinking. Often the effects are pleasurable, but its high potency can make it difficult to take the drug safely, as just a few milligrams can have a large impact on the experience.
Compared to a dissociative like ketamine or methoxetamine (MXE), it is typically more energizing. This can be positive at low to common doses because people find it easier to engage in daily activities and they may even be more motivated to be active, but it also makes high-dose experiences riskier because a user may not reliably lie down even when they are very impaired.
3-MeO-PCP also induces hypomanic- and manic-type effects that can be enjoyable at smaller doses—due to increased mood, confidence, energy, etc—yet can easily be dangerous at higher doses and in vulnerable people. As these effects increase, delusions can readily occur, potentially leading to injury, self-harm, risks to nearby people, and property damage.
Article PDF: Link
Synonyms
3-Methoxyphencyclidine = 3-MeO-PCP
IUPAC: 1-[1-(3-methoxyphenyl)cyclohexyl]piperidine
Other information
PubChem ID: 11778080
Molecular formula: C18H27NO
Molecular weight: 273.4 g/mol
Contents
Section 1: Routes of Administration, Timeline, and Dose
Potency warning
This drug cannot be dosed safely without a milligram scale and because of its potency, volumetric dosing is required when using a standard consumer-grade scale. Although these scales provide readings at the milligram level, they are not accurate at that level. Therefore, a larger amount should be weighed, such as 100 mg, and then dissolved in an appropriate solvent.
For example, 3-MeO-PCP could be dissolved in a solvent at a concentration of 5 mg/mL and then an oral syringe could be used to accurately dose the drug based on volume.
Irritation warning
Whether this is batch-specific is unclear, but some users find it irritating to sensitive areas when using routes of administration (ROA) that involve extended contact with the drug. Users have reported discomfort and possibly some temporary tissue damage in the nose and rectum, as well as in the mouth when taken sublingually.
Differences between ROA
Oral use tends to produce more dissociation, confusion, and impairment. Intranasal use may cause more stimulation and a somewhat clearer headspace, though potentially with more mania. These distinctions become less important as the dose increases, as each ROA can produce strong dissociative effects when enough is used.
Because of the intranasal effect profile and the kinetics of that ROA (i.e. faster onset, wearing off sooner), compulsive redosing may be more likely with intranasal administration.
Oral
The dose range encompassing the largest number of positive and relatively safe experiences is ~5 to 15 mg. Users should try light doses first and slowly increase the amount during subsequent experiences because relatively small doses can be intense for some users.
Compared with many drugs, the oral onset time is slower, and people may be minimally affected until ~90 min has passed, though some report effects a bit earlier. Because of the slow onset, it is very important to avoid redosing based on feeling the effects are inadequate during the first two hours.
Doses
- Light: 2 – 4 mg
- Common: 5 – 12 mg
- Strong: 13 – 17 mg
Timeline
- Onset: 45 – 90 min
- Total: 5 – 8 hours (this can extend to 12+ hours with high doses and/or redosing)
Intranasal
The onset is faster than with oral use, but still slower than may be expected. It is best to avoid redosing until at least 45-60+ min has passed.
Comfort
Several users have described it as feeling caustic and producing pain, a burning/stinging sensation, and rhinorrhea (runny nose) for some. Bleeding may occur, but the risk is fairly low unless you are already experiencing nasal irritation or are repeatedly using 3-MeO-PCP.
Others have reported it is relatively easy to insufflate and not especially uncomfortable compared with some drugs. Inconsistent reports may indicate variable product purity, but that is currently unknown. Those who report it is painful to insufflate may still find it becomes numbing once multiple doses are used, and those who find it less uncomfortable have sometimes reported it is numbing with a single dose.
Doses
- Light: 2 – 4 mg
- Common: 5 – 10 mg
- Strong: 11 – 15 mg
Timeline
- Onset: 10 – 35 min
- Total: 4 – 7 hours
Rectal
There are far fewer reports of rectal use, so the dosing and timeline information is not reliable enough to specify. It should be treated as having a slightly higher potency than oral administration, the onset may be faster (i.e. closer to 20-45 min), and the duration is between that of oral and intranasal administration.
Overall, the effect profile seems to be closer to oral than to intranasal, but with faster kinetics.
Section 2: Effects
2.1 Introduction
Overview
The core effects include a dose-dependent disconnection from your senses—e.g. choppy and distorted vision, numbness, and impaired taste and smell—and from your body. Because of these properties, users may feel as though they are no longer identical with their body and are instead riding around in a sort of vehicle or robot. Further, a user’s mind can seem as if it is physically positioned somewhere behind the body such that they are watching or controlling the body in a videogame-type manner.
The effects depend on the user, the dose, and the individual experience. Some experiences are characterized by a cold, emotionless, anhedonic (deficit in the ability to feel pleasure), and detached state. Yet in other cases, the drug is euphoric, anxiolytic (anxiety reducing), energizing, disinhibiting, and hypomanic.
Individual users have described it as confusing, wonderful, terrifying, and enjoyable, reflecting the wide range of effects it can produce in a single person.
Among those who have very positive experiences, it is still common for the effects to vary between experiences and slightly different doses. Those who feel great on it one day may feel cold and detached another day. This unpredictability turns some users off the drug and makes it difficult for people to have a straightforward opinion about it. A few milligrams can drastically alter the intensity, which may contribute to the variable effects, particularly since many users do not dose the drug volumetrically and are therefore unlikely to know how much they have used.
At doses that lack significant hypomanic-type effects, even if anxiolysis and moderate mood enhancement are present, the experience may be boring relative to psychedelics, for example. This is partly why many users combine the drug with some kind of activity, such as social interaction or physical activities, rather than sitting around. Some users find it boring in one situation (e.g. at home by themselves), yet fun upon changing the environment and activity. When intending to be out in public, only light to common doses should be taken and users should first be acquainted with the effects in private. And regardless of a user’s confidence about their ability to feel comfortable while altered in public, the effects of 3-MeO-PCP are difficult to predict and the experience can easily become confusing and uncomfortable around more people.
Positive
- Dissociation
- Mood enhancement
- Anxiolysis
- Increased sociability (mostly at low to common doses)
- A hypomanic-like state that may include excessive confidence (e.g. in oneself and in unwise ideas and plans), high energy, the belief that one has special knowledge about things, and recklessness
- Analgesia (pain relief)
- Visual distortions, primarily of depth perception, acuity, and the shape/size of objects
Negative
- Heart rate (HR) and blood pressure (BP) increase
- Mania
- Delusions
- Psychosis
- Tinnitus (ringing in the ears)
- Disorientation
- Dizziness
- Anxiety and panic
- Cognitive impairment
- Distressing feelings of emotional detachment and anhedonia
- Confusion
2.2 Mental, Cognitive, and Perceptual
Functionality
A common descriptor for 3-MeO-PCP is “functional” because light to common doses can permit normal activities to a greater degree than many other dissociatives, and users are more inclined to engage in those activities due to its energizing effect. It is certainly true that with relatively small doses, people can be physically active, communicate with others, and almost feel as though they have not taken a dissociative, but this can also cause people to overestimate their capabilities. The feeling of “functionality” can be insidious because it contributes to the belief that one can take low doses on a regular basis as part of their daily routine, akin to how some people head down a risky path by frequently “enhancing” their daily life by using opioids or benzodiazepines.
Those looking for a ketamine-type experience may not find value in the relative functionality of the drug. After all, being able to do daily tasks is not usually what people have in mind when they take a dissociative. But for others, light to common doses are preferable to strong doses precisely because of the unique, minimally dissociative effects.
A related descriptor that is also frequently used is “clearheaded.” This can be an appropriate characterization at low doses, but as the dose increases, there is a very good chance that the feeling of clearheadedness is a trick. In reality, a user may be impaired, manic, and/or delusional, yet they subjectively feel as though they are thinking straight, and perhaps thinking even more clearly than when sober. Connected to this, people’s overall perception of how altered they are can be very different while on the drug, so it is common for users to only realize how substantial the effects were retrospectively.
The minimal or at least acceptable degree of impairment at light to common doses can make creative endeavors worthwhile, such as working on music, art, and writing. Depending on the person, somewhere in the common to strong dose range, creative activities may still be rewarding but they can also become more difficult.
Mania and delusional thinking
Positive experiences often include hypomanic-like effects, such as increased confidence, more motivation, feeling like one has insight into things (e.g. the universe, other people), heightened mood, and jumping around to different activities and tangential ideas and plans. The important thing is that although the ideas may be ridiculous and the plans may be a bit foolhardy, users are not so detached from reality as to be at a high risk of self-harm or harming others, and they may remain capable of functioning in the world. Nevertheless, this remains an inherently risky state to be in because the delusions of grandeur and delusions of sobriety associated with 3-MeO-PCP can quickly become dangerous.
The hypomanic-type thinking can include a user believing they have amazing ideas, are great in social settings, and can do just about anything with high proficiency. Usually those beliefs do not line up with reality, and if the user is in a social situation, they run the risk of being annoying and embarrassing themselves.
Effects like these are not universal and they are very dose-dependent. When these effects are not prominent, the user may just feel excessively impaired and dumb, not like an enlightened being. They may also feel more disconnected from the world, rather than in touch with the world and with other people.
With higher doses, prolonged redosing, and frequent use, mania and detachment from reality become more likely. Users may firmly believe their delusions and once they have a delusional belief—one that could involve a plan that the user must follow—the resultant behaviors could be destructive and dangerous. And if those behaviors are applied to oneself or outward towards others, they can involve self-harm or violence.
Users may feel a sense of power, either in the form of thinking they are remarkably intelligent and have access to knowledge that others lack, or in the form of power over reality (e.g. controlling time, reading minds).
High doses can also simply produce weird experiences that despite involving delusions, mania, or irrational behavior may not be harmful. Examples include someone crawling around their house believing they are teleporting or going back and forth through time, or someone who makes the poor decision to move around everything in their room because they dropped an insignificant item and are trying to find it.
When someone loses their connection to reality, it is common for them to feel more in control due to hypomania and mania. But it is also possible to become paranoid and to feel targeted by a malevolent force or plot, making the experience uncomfortable. Some users become paranoid and terrified because they feel like they are going insane.
It cannot be stressed enough that many users wind up dealing with the police, being taken to an emergency department, damaging property, and/or causing a disturbance upon losing control at high doses or during binges. Users have described losing track of hours only to emerge with injuries, lying in a hospital, or having a lot to explain to their friends and family. The impact of an overly intense experience can often be more consequential than that of a difficult psychedelic experience, for example, where the typical consequences are anxiety and stress.
Introspection
Non-delusional introspection can occur, most often with common doses. Users have described thinking about their lives (e.g. mistakes, upcoming choices, recent hardships, prospects), their friends and family, and their society. This can produce genuinely positive effects that persist beyond the experience, as with psychedelics, though more often people will either not experience meaningful insight or they will engage in introspection but not implement any of their insights once sober.
Energy
3-MeO-PCP is more energizing than a dissociative like ketamine. The character of the stimulation is not necessarily the same as that of classic psychostimulants (e.g. amphetamine, cocaine), but users often feel they need to be active and moving around, or they at least have the ability to do so. People may pace around and at the appropriate dose (usually light to common), they may enjoy physical activities.
Multiple users have specifically mentioned enjoying physical activities outdoors, such as walking, cycling, or mountain biking. With an activity like cycling, even though it is not as risky as driving, impairment still matters, particularly when one is around other people and traffic. It is wise for users to stick with lower doses and to remain in areas that are safe in case they are more impaired than they realize, i.e. do not go cycling in a high-traffic location.
The energizing property has also been used for exercise, such as for resistance training or bodyweight exercises like pushups. It may increase time to fatigue and make the exercises feel easier than normal. After all, users are functioning while partially anesthetized. While this may be acceptably safe for simple bodyweight exercises at light to common doses, adding weights to the mix while on a drug that can impair balance, coordination, and perception of strain on the body is not a good idea.
The increase in exercise capacity is essentially an illusion. Rather than being capable of doing more work, a user does not realize when they are overexerting, which may result in injury. Likewise, yoga and stretching are sometimes reported to feel nice, but users should be careful not to push those movements much beyond their normal capacity, no matter how it feels.
A hectic presentation of the increase in energy and desire to do things may occur. Users have reported jumping from task to task and excessively cleaning or organizing, akin to how people on classic psychostimulants can behave.
While frequently energizing and thereby restlessness-inducing, physical energy is not always prominent and it may be less important at higher doses, so it is good to have the option of relaxing somewhere. Another possibility is that high doses can make physical activities more difficult, but the sensation of energy remains—as such, a user can feel restless when not moving around, even though they also cannot do much when they try to move around. This contributes to the safety concerns with high doses, as people may be inclined to be physically active when it is unsafe to do so, considering the risk of accidental injury.
Anxiety and disinhibition
Anxiolysis may occur and users have reported feeling disinhibited in social settings, i.e. it reduces social anxiety for many users and can make them more inclined to do things. Because of these effects, 3-MeO-PCP has been likened to the experience of a few drinks of alcohol, at least early in the effect period.
This is best experienced at light to common doses because any experience that is intense or confusing can trigger anxiety and panic. Those looking for anxiolysis and increased sociability should try light doses, which may reduce anxiety with minimal concurrent impairment and with few effects aside from energy, anxiolysis, and disinhibition.
If a user receives these positive effects from a light dose, that does not mean more is better. One should be careful not to make the mistake of redosing or taking larger amounts in the belief that it will enhance the effects—it may very well do the opposite.
Sociable doses are described by some as superior to alcohol and benzodiazepines, but users must carefully experiment with small doses until they find the amount that works, and it is unlikely to provide these effects for everyone.
Mood
The range of effects on mood encompass euphoria, complete detachment from emotions, and depression. Due to the variability, it is possible that reports of mood enhancement and euphoria partly depend on (i) anxiolysis and disinhibition, and/or (ii) hypomanic effects. With the former, this could make 3-MeO-PCP somewhat comparable to benzodiazepines in that substantial mood enhancement is not a reliable effect of the drug, yet it can occur in those for whom anxiety and stress reduction are highly liberating.
Antidepressant
The dissociative ketamine is a well-validated, rapid-acting antidepressant and other dissociatives, such as dextromethorphan (DXM), may have similar properties. With 3-MeO-PCP, not enough users with depression have reported their experiences and therefore it is unknown whether an antidepressant effect in the days following the experience should be expected.
A few users have reported rapid antidepressant effects, but a handful of reports is not very insightful. Regardless of whether someone has depression or not, it can produce a 1-2 day afterglow consisting of effects like elevated mood, reduced anxiety, a positive outlook, and increased energy. However, that afterglow is distinct from the 3-7 day antidepressant effect of ketamine.
Cognitive impairment
With common to strong doses, users should expect to struggle with complicated daily tasks and they will very likely have memory impairment. People often forget what they were intending to do, are unable to follow along with conversations or the plot of movies and television shows, and more generally lose track of what is going on even at the scale of seconds to minutes.
Users may be unable to fully remember earlier parts of the experience. For example, someone can get started on an activity or become immersed in music for an hour, then struggle to recall what they were doing prior to that activity.
At strong+ doses, people may not understand what is going on or know where they are, which can trigger significant anxiety. Having a sober, trusted friend present is a good idea as they can provide reassurance in these situations.
Unconsciousness
Rarely will someone become unconscious for the duration of the effects. Even very large doses (e.g. >50 mg) often permit being awake, albeit highly impaired with amnesia for portions of the experience. Some users report “waking up” partway into the experience, but they are typically using the drug alone with no one to witness what they had been doing, so it is possible they have amnesia for the period in which they think they were unconscious.
Unconsciousness is possible, particularly with large doses, but it should not be expected.
Holing and visual disconnection
The standard view is that you cannot hole on 3-MeO-PCP, meaning people do not enter a state of full disconnection from vision that enables a hallucinatory (“out of body”) state to take over, whether eyes are open or closed. This is at least largely true and more importantly, people should not try to reach such a state on this dissociative.
Strong+ doses will more often yield a manic, psychotic, and/or delusional state in which the user can be a danger to themselves or others. Physical immobilization is not a standard effect of 3-MeO-PCP, therefore when someone is greatly altered and exerting minimal conscious and rational control over their body, they can still act out instead of just lying down.
Some users report closed-eye experiences in which they see memories, landscapes, shapes, and patterns. They may feel detached from their body when their eyes are closed, no longer noticing any distinction between themselves and the surrounding space, creating a sensation of floating or of no longer being embodied.
Visual perception
At light and lower-common doses, it is not a notably visual drug and in general, it should not be expected to produce anything like a psychedelic experience. Instead, the primary open-eye visuals are distortions of size, distance, clarity, etc. Things may appear much closer or farther, as well as smaller or larger. And the effects can vary between items, with some appearing very large and close while others appear small and distant, for example. Reduced visual acuity is often reported with common to strong doses, leaving one’s visual field less clear.
Some of the more psychedelic-like effects include things appearing brighter and an intensification of colors, perhaps more often experienced with light to common doses. With strong doses, some warping of the shape of items can occur.
Auditory perception
There can be a dose-dependent interference with auditory perception. Things may sound more distant, muffled, tinny or “mechanical,” and generally of reduced quality. As such, music may be distorted in a way that essentially makes all genres unenjoyable and the distinctions between genres may be less apparent. However, as with many aspects of the drug, this is dose-dependent and subject to individual variation. Especially with light to common doses, many users find music more enjoyable and engaging.
Tactile, olfactory, taste, and bodily perception
With light to common doses, which typically do not cause severe physical impairment, it is common to feel as if one’s body is significantly lighter and as if one’s limbs are almost weightless when they are moved. With the increase in physical impairment caused by higher doses, these effects can be overridden by the feeling that it is more difficult to move one’s body.
Tactile perception is impeded dose-dependently such that common to strong doses often produce a numbing effect. Likewise, analgesia (pain relief) is common. But with smaller doses, some users experience tactile enhancement where things feel softer and smoother, for example.
As with the other senses, olfaction (sense of smell) and taste will usually be impeded dose-dependently.
Time perception
Time distortion is frequently reported with common to strong doses. Distortion usually presents as time dilation, i.e. events seem to occur more slowly than they are. Users may feel like a simple activity, such as sending a message or walking to another room, took longer than it did. This can be coupled with a general sensation of everything in the world being slowed down.
Redosing
Risky and compulsive redosing are a problem for some users, especially with common to strong+ doses and when people do not have a preexisting plan for how much they are going to take. Partly because of its tendency to induce overconfidence and overenthusiasm, someone may decide to redose even when that was not their original plan.
Further, when large doses are taken, the user may take more while delusional and confused. This often ends poorly, as redosing is one of the most important factors linked to experiences that end up involving interactions with the police, property damage, and trips to the hospital.
Because of the risk that one could redose while highly impaired and irrational, it is best for the user to pre-prepare their doses and then store away the rest, either with a friend or at least somewhere that would be difficult to access under the influence.
Just because a user can feel like they are thinking clearly and are overflowing with “great” ideas and confidence (owing to their hypomania/mania) does not mean redosing is wise. Usually it is not.
2.3 Physical
Bodily sensations
A potentially pleasant sensation of energy or vibration throughout the body may occur.
Cardiovascular, chest, and palpitations
Mostly at higher doses, some users report feeling like they have an excessively high heart rate or that their chest is tight. Based on the plentiful research on PCP and ketamine, along with a smaller amount of 3-MeO-PCP literature, the drug likely induces a moderate increase in heart rate and blood pressure.
Only a fraction of users become focused on sensations potentially associated with these physiological effects. Anxiety and panic increase the likelihood of turning one’s focus to these sensations, even when they are not linked to any physiological effect. Hyperfocusing on sensations like heart palpitations can then further exacerbate anxiety.
Speaking
Speaking often becomes difficult, primarily with common to strong doses. It can cause slurring and users may feel a generalized lack of control over their mouth. Tongue numbness likely contributes to how odd it can feel when attempting to speak on sufficiently intense doses.
Coordination and motor effects
At low to common doses, objective impairment will dose-dependently occur and high-risk activities like driving should be completely avoided. The impairment may be more difficult to notice subjectively. If the dose is low, usually the impairment will not be severe enough for simple actions like walking to become dangerous and a user may not feel unsteady.
The risk changes significantly at common to strong doses, as these can cause incoordination, imbalance, and other impairments that make walking and other movements feel strange and difficult. Sometimes the perceived impairment is greater than the objective impairment. Since the drug radically alters one’s perception of their body, they may think they are moving more unusually than they are. Both real and perceived impairment readily occur as the dose increases.
2.4 Aftereffects
Acute
If a low dose is taken early in the day, the user may return to normal by evening. Otherwise, people commonly feel somewhat altered until they have slept and woken up the following day, even if the core drug effects wore off hours before sleep. Typical acute aftereffects include cognitive impairment, bodily numbness and/or lightness, reduced visual acuity and depth perception impairment, and insomnia. So long as light to common doses are taken, insomnia may only last a few hours beyond the main effect period.
Larger doses and doses taken closer to sleep may cause sleep to be less restorative than normal because the lingering influence of low levels of the drug could prevent naturalistic sleep.
Day after
How one feels the day after using 3-MeO-PCP strongly depends on when it was used and how much was taken. With moderate doses that have not substantially interfered with sleep, there may be an afterglow consisting of better-than-usual outlook and perspective, enhanced mood, and anxiolysis. Not everyone experiences an afterglow, but so long as moderate amounts are used at a reasonable time, users typically will not experience substantial negative effects the following day.
Especially if the drug is taken late in the day, sleep is interfered with, and/or large doses are used, one may wake up with cognitive impairment (e.g. brain fog; not feeling as sharp; memory impairment), vision impairment (e.g. blurriness), lingering dissociation, and a general hangover feeling. The hangover and other aftereffects from a single dose will typically decline by afternoon.
2.5 Chronic Use
Desire to keep using
Unlike many dissociatives, certain doses of 3-MeO-PCP at least seem to permit engaging in daily activities, including work—granted, a user is likely still impaired enough that they cannot safely engage in high-risk activities like driving and operating heavy machinery.
Lower doses can be mood enhancing, stimulating, and motivating, which has caused many people to use it daily or on most days. Some report a large reduction in anxiety and depression, coupled with greater interest in activities (both boring and fun), and heightened confidence in their capabilities, sometimes even coming with a desire for self-improvement. Indeed, there are reports of people feeling so alive and engaged with the world that they become committed to exercising more, pursuing work and education opportunities, etc.
While it can seem beneficial in the initial days or weeks of frequent low-dose use, this is a very risky way to take the drug and it almost always ends poorly. The number of people who describe it as “amazing,” “the best,” and “life-changing” in the context of enhancing their day-to-day mental state is concerning. Some describe it as feeling like they are “themselves, but better” or like they are consistently having the best sober day of their life, yet those experiences are deceptive.
Self-evaluations of the drug can be deceptive in at least a couple ways. First, one may genuinely feel better in a non-delusional way, yet if they continue with their use it will usually result in mood dysregulation, unusual behavior, mania, psychosis, and/or delusions. Second, positive self-reports can be tainted by hypomania, causing people to believe the drug is more effective and benign than it really is, sometimes generating the belief that it is the cure for all of their mental ailments.
The effects become detrimental at different times for each user. Some people begin losing touch with reality within a week of daily use, while others use it for a few months before stopping. Early on the reports are glowing, but users often voice the opposite opinion about the drug once it becomes obvious that it is damaging for their mental state.
Compulsive and irrational redosing can be a problem while on the drug, but normally it does not produce significant compulsions when sober. Once people stop taking 3-MeO-PCP, the urge to return to use is smaller than with drugs classically associated with addiction.
Mania, psychosis, delusions, and mood
Using it for days, often without adequate sleep, greatly increases the risk of mania and psychosis. Light to common doses that do not acutely produce mania or psychosis can cause those problems when taken day after day.
For example, someone using 5-10 mg daily can find themselves slowly slipping into manic and delusional thought patterns over a period of weeks or months. The unusual thought patterns may begin as odd ideas that the user can ignore, but if use persists, those thoughts tend to become more complex, more persistent, and harder to ignore. Eventually, people may act out in accordance with those irrational and delusional thoughts, which can be dangerous.
With frequent use, particularly over a period of weeks or longer, mood dysregulation can occur. 3-MeO-PCP may initially cause consistent mood enhancement, but over time that can transition to an unstable mood, with users oscillating unpredictably between mood elevation and depression. Likewise, one can be very emotional at one moment and dissociated the next. It can also trigger irritability.
Section 3: Chemistry
3.1 Overview
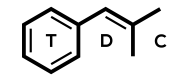
3-MeO-PCP is a methoxylated derivative of phencyclidine (PCP). Both are in the arylcyclohexylamine class of dissociatives. Their primary constituents are a cyclohexane ring, a heterocyclic nitrogen-containing piperidine ring, and a phenyl ring. 3-MeO-PCP only differs from PCP by the substitution of a methoxy group at carbon #3 of the phenyl ring. This substitution slightly increases potency, whereas methoxylation at carbon #4 of the phenyl ring (i.e. with 4-MeO-PCP) greatly reduces potency.
3.2 Immunoassays
3-MeO-PCP can cross-react with immunoassays for PCP, producing false-positives.
In a cloned enzyme donor immunoassay (CEDIA) for PCP, the cross-reactivity was 14.5%, meaning 175 ng/mL 3-MeO-PCP gave a result akin to that of ~25 ng/mL PCP (Backberg et al., 2015). As such, these tests may be less sensitive in detecting 3-MeO-PCP, but recent drug use will often yield concentrations large enough for a positive result.
Backberg and colleagues tested 53 urine samples known to contain 3- and/or 4-MeO-PCP, and 45 (85%) tested positive in an immunoassay for PCP (cutoff: 25 ng/mL) (Backberg et al., 2015). Positive samples contained a mean drug concentration of 5,093 ng/mL (range: 21 – 52,759 ng/mL). Low concentrations of 3-MeO-PCP (4-60 ng/mL) were present in the samples that gave a negative result. The positive results may have involved contribution from 3- and 4-MeO-PCP metabolites, not just parent drug.
Cross-reactivity with PCP screening has also been reported in multiple case reports (Bakota et al., 2016; Mitchell-Mata et al., 2017; Thornton et al., 2017; Zidkova et al., 2017; Chang and Smith, 2017).
Section 4: Pharmacology
4.1 Overview
3-MeO-PCP has a high affinity for N-methyl-D-aspartate receptors (NMDARs) and interacts with the same region of those protein complexes targeted by other dissociatives like ketamine and PCP (Roth et al., 2013, 2018; Mitsuoka et al., 2019). Aside from binding data and evidence that it functions as an NMDAR antagonist, more detailed information about its interaction with NMDARs is unavailable. It likely functions as an open-channel, voltage-dependent, uncompetitive antagonist. This means it binds inside NMDARs when the neuronal membrane voltage begins to shift, releasing the magnesium ions that block most, though not all, NMDAR channels near the resting membrane potential.
Despite claims about it having dopaminergic and opioidergic properties, the evidence indicates this is incorrect. The research is not settled and some findings are conflicting, but the available research is largely consistent with regard to these proposed effects. Roth et al. (2013, 2018) detected no meaningful interaction with mu-opioid (MOR) and kappa-opioid receptors (KOR) nor dopamine receptors and the dopamine transporter (DAT). The same was reported by Wallach (2014, as cited in Wallach and Brandt, 2018), except for a high affinity for the kappa-opioid receptor.
Beyond NMDARs, the drug interacts with sigma-1 (σ1) and potentially sigma-2 (σ2) receptors, as well as the serotonin transporter (SERT) (Roth et al., 2013, 2018; Wallach, 2014 as cited in Wallach and Brandt, 2018).
3-MeO-PCP is tentatively estimated to have a half-life of 10 to 11 hours (Backberg et al., 2015; Johansson et al., 2017). The dissociative 3-HO-PCP appears to be a major metabolite and because it is similarly potent, it may contribute to the effects. 3-HO-PCP has been detected in human fatality cases and in vitro (Michely et al., 2017; Ameline et al., 2019; Bakota et al., 2016).
4.2 Pharmacodynamics
Interactions with central nervous system receptors were studied as part of the Psychoactive Drug Screening Program (PDSP) operated by the University of North Carolina at Chapel Hill and the National Institute of Mental Health (NIMH). Out of 57 targets, 3-MeO-PCP was found to inhibit radiolabeled ligand binding by ≥50% at the histamine H1 receptor, NMDA receptor (NMDAR), serotonin transporter (SERT), and the sigma-1 receptor (σ1R) (Roth et al., 2013, 2018). The affinity (Ki) values were:
- NMDAR = 20 nM
- SERT = 216 nM
- σ1R = 42 nM
- H1R = 2960 nM
For comparison, these were the interactions identified for other dissociatives tested by Roth et al. (2013, 2018):
- 4-MeO-PCP
- Norepinephrine transporter (NET; 713 nM), NMDAR (404 nM), SERT (844 nM), σ1R (296 nM), σ2R (143 nM)
- 3-MeO-PCE
- α2A (964 nM), DAT (743 nM), H2R (2097 nM), NMDAR (61 nM), SERT (115 nM), σ1R (4519 nM), σ2R (525 nM)
- Ketamine
- NMDAR (659 nM)
- PCP:
- NMDAR (59 nM), SERT (2234 nM), σ2R (136 nM)
- MXE
- NMDAR (259 nM), SERT (481 nM)
Another study found similar interactions with NMDAR for PCP and 3-MeO-PCP using cultured neurons sourced from the hippocampi of Wistar rats (Mitsuoka et al., 2019). This research assessed interactions with NMDAR based on how the drugs affected glutamate-induced changes in the level of drebrin, a protein involved in dendritic spine maturation. Activation of NMDARs by glutamate causes drebrin exodus, and NMDAR antagonists inhibit that process. 3-MeO-PCP inhibited glutamate-induced drebrin exodus with an IC50 of 1.51 μM, compared with 2.02 μM for PCP.
Some of the results reported by Roth et al. (2013, 2018) differed from those of Wallach (2014, as cited in Wallach and Brandt, 2018). The Ki differences include:
- Data from Roth et al. (2013, 2018)
- NMDAR: 20 nM
- NET: >10,000 nM
- SERT: 216 nM
- σ1R: 42 nM
- σ2R: >10,000 nM
- MOR: >10,000 nM
- KOR: >10,000 nM
- Data from Wallach (2014, as cited in Wallach and Brandt, 2018)
- NMDAR: 38.1 nM
- NET: 1,808 nM
- SERT: 1,571 nM
- σ1R: 436 nM
- σ2R: 154.4 nM
- MOR: 9,418 nM
- KOR: 168.8 nM
Astrand et al. (2020) tested the activity of 3-MeO-PCP using cell lines expressing human MOR, CB1, 5-HT2A, and 5-HT1A receptors. The only interaction was with MOR, where it activated the receptor at a concentration of 7.5 μg/mL (~27.5 μM), and the signal intensity was less than 50% of a full agonist.
An early pharmacodynamic study using rat brain homogenate found the IC50 of 3-MeO-PCP for inhibiting the binding of labeled PCP was 90 nM, which should largely correspond to its interaction with NMDARs (Vignon et al., 1982). In mice, the ED50 for inducing impairment in the rotarod test (i.e. causing mice to fall off) was 4.8 mg/kg. For comparison, the ED50 of PCP was 4 mg/kg.
The ED50 for rotarod impairment was similar in separate experiments performed by Wallach (2014, as cited in Wallach and Brandt, 2018). With IP administration, the ED50 in male CF-1 mice was 5.2 mg/kg, and the oral ED50 was 11.29 mg/kg. 3-MeO-PCP also produced minimal motor impairment in male Sprague-Dawley rats with an IP ED50 of 5.94 mg/kg and an oral ED50 of 15.3 mg/kg.
In the maximal electroshock seizure (MES) test, it inhibited tonic limb extension in male CF-1 mice and male Sprague-Dawley rats with the following ED50: mice (IP = 3.2 mg/kg; oral = 6.6 mg/kg) and rats (IP = 4.05 mg/kg; oral = 3.2 mg/kg) (Wallach, 2014, as cited in Wallach and Brandt, 2018). 3-MeO-PCP was protective against metronidazole-induced seizures, providing partial protection in mice at 20 mg/kg (oral) and its oral ED50 in rats was 9.4 mg/kg. When given larger doses, mice were sedated at 100 mg/kg (IP) and some died at 100 and 300 mg/kg.
Vignon et al. (1988, as cited in Wallach and Brandt, 2018) found 3-MeO-PCP inhibited dopamine uptake into rat brain synaptosomes with an IC50 of 490 nM, similar to PCP (IC50 = 500 nM).
4.3 Pharmacokinetics
Elimination Kinetics
A couple case reports have included enough data to roughly estimate its half-life. Johansson et al. (2017) reported a case in which four blood samples were taken during the course of treatment and based on the change in concentration over time, the half-life was estimated to be ~11 hours, assuming typical first-order elimination kinetics. Using samples from a case enrolled in the Swedish STRIDA project where the blood concentration decreased from 73 to 30 ng/mL over an 11-hour period, Backberg et al. (2015) estimated the half-life to be ~10 hours.
Metabolism
The metabolism of 3-MeO-PCP was studied by Michely et al. (2017) using rats and human liver microsomes (HLM). In rats, 30 phase I metabolites and seven phase II metabolites were identified in urine after they received 3-MeO-PCP at 10 mg/kg enterally. The metabolic pathways involved hydroxylation at the cyclohexyl and/or piperidine rings, and O-demethylation, which could then be followed by hydroxylation. All seven phase II metabolites were glucuronides.
Incubation with HLM produced some of the metabolites identified in rat urine, with the metabolic processes including O-demethylation, piperidine-hydroxylation, and cyclohexyl-hydroxylation (Michely et al., 2017). Hydroxylation at the cyclohexyl and piperidine rings was largely attributed to CYP2B6 with some contribution from CYP2C19 for piperidine hydroxylation, while O-demethylation was catalyzed by CYP2C19, CYP2B6, and CYP2D6.
Ameline et al. (2019) reported additional metabolic information from two fatalities discussed by Grossenbacher et al. (2019). First, the researchers incubated the drug in vitro with human liver microsomes, yielding these metabolites: O-demethyl-3-MeO-PCP; piperidine-hydroxy-3-MeO-PCP; O-demethyl-piperidine-dihydroxy-3-MeO-PCP; piperidine-dihydroxy-3-MeO-PCP; and cyclohexyl-hydroxy-piperidine-dihydroxy-3-MeO-PCP.
Four of the five metabolites detected in vitro were present in urine from both fatalities: O-demethyl-3-MeO-PCP, piperidine-hydroxy-3-MeO-PCP, O-demethyl-piperidine-dihydroxy-3-MeO-PCP, and piperidine-dihydroxy-3-MeO-PCP (Ameline et al., 2019). The metabolites were not quantified, but the ratio of metabolite to parent drug was determined based on peak area, providing some insight into the relative abundance of each. O-Demethyl-3-MeO-PCP had 69% of the parent drug peak area, piperidine-hydroxy-3-MeO-PCP was 25%, O-demethyl-piperidine-dihydroxy-3-MeO-PCP was 7%, and piperidine-dihydroxy-3-MeO-PCP was 7%. The authors note that metabolite detection may not lengthen the window of detection in intoxication cases because every metabolite had a ratio less than 1, suggesting they may not persist longer than 3-MeO-PCP. Notably, O-demethyl-3-MeO-PCP is also known as 3-HO-PCP, a similarly potent dissociative. 3-HO-PCP appears to be a major metabolite and could be expected to contribute to the effects.
3-HO-PCP was also tentatively identified by Bakota et al. (2016) in blood from a 29-year-old male who died with 3-MeO-PCP and other drugs in his system. The identity of the peak corresponding to 3-HO-PCP was not confirmed because a standard for that substance was unavailable. Also, because the powder found near the decedent was never tested due to an oversight, it is possible that the decedent used both 3-MeO-PCP and 3-HO-PCP, rather than the apparent 3-HO-PCP arising from metabolism.
Zidkova et al. (2017) analyzed urine from two intoxication cases and tentatively identified three peaks as corresponding to hydroxylated piperidine and cyclohexyl metabolites.
Section 5: History
After Maddox et al. (1965) reported the synthesis of 2-MeO-PCP and 4-MeO-PCP as part of an investigation into potential CNS depressants, Geneste et al. (1979, as cited in Morris and Wallach, 2014) synthesized 3-MeO-PCP. For two decades, the drug was confined to occasional scientific research, such as investigations into its pharmacology (Vignon et al., 1982; Wallach and Brandt, 2018).
John Q. Beagle, a pseudonymous member of the online drug forum The Hive, first described the effects of 3-MeO-PCP in 1999 (Beagle, n.d.). According to Beagle, the drug produced effects that were “extremely similar to PCP in potency and quality.”
It was not until the 2010s that 3-MeO-PCP began to gain a real foothold in the research chemical market. As discussed by Morris and Wallach (2014), one of the earliest reports about 3-MeO-PCP came in 2009 from Bluelight.org user ‘hugo24’ (Bluelight, 2009). By April 2011, online vendors like Buy Research Chemicals UK (BRC) were selling it and the number of vendors increased concurrent with a growing number of experience reports, many of which were positive (Morris and Wallach, 2014).
Data from 84,678 threads was collected from Drugs-Forum.com (specifically the “Drugs Information and Harm Reduction” section) to gauge the popularity of novel drugs over time, revealing 3-MeO-PCP first appeared on the forum around 2011, peaked in popularity between 2011-2013, and was no longer discussed enough to be considered “present” on the forum by early 2016 (Rhumorbarbe et al., 2019).
3-MeO-PCP was first notified to the EU’s Early Warning System (EWS), which is operated by the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) and Europol, in March 2012 by the UK (EMCDDA-Europol, 2013).
It was first detected by Sweden’s STRIDA project in 2013, according to an analysis of 2626 suspected NPS intoxication cases enrolled in the project between January 2010 and February 2016 (Helander et al., 2020). The drug was detected in 2013 (Quarter Four; Q4), 2014 (Q1-4), and 2015 (Q1-2). 3-MeO-PCP became regulated in Sweden in Q2 2015 and it was not detected by STRIDA through the rest of the data collection period in 2015 and early 2016.
Fatalities began appearing by the mid-2010s. The EMCDDA received notice of three deaths associated with 3-MeO-PCP in Sweden in October 2014 (EMCDDA-Europol, 2015), which were among the earliest fatalities on record.
Backberg et al. (2018) analyzed 251 drug products from 173 cases of suspected NPS intoxication as part of the Swedish STRIDA project between 2010 and 2015. 3-MeO-PCP was present in seven products, which were submitted in 2013, 2014, and 2015. Those products were powders and liquids. Additionally, two products (a tablet and a liquid) submitted in 2014 contained either 3-MeO-PCP or 4-MeO-PCP. In one case, the product’s label or the user’s self-report indicated the product was 3-MeO-PCP, yet flubromazolam was the primary drug instead. 3-MeO-PCP was identified in a few products that contained multiple drugs, including:
- N-Methyl-N-ethyltryptamine (MET) product that contained MET as the primary NPS content, with trace levels of 3-MeO-PCP/4-MeO-PCP, 4-AcO-DMT, 3-MEC, and 4F-α-PVP. The product also contained ketamine.
- 3-MeO-PCP product that contained flubromazolam as the primary NPS content, with trace levels of 4F-α-PVP and 3-MeO-PCP/4-MeO-PCP. The product also contained indigo and caffeine.
- 4-MeO-PCP product that contained 4-MeO-PCP as the primary NPS content, with 3-MeO-PCP as a minor component.
A survey of Bluelight.org users conducted between November 2014 and February 2015 investigated their NPS use (Soussan and Kjellgren, 2016). There were 619 respondents (517 males, 102 females; mean age: 27.6 years) who collectively used 177 different NPS, with 3-MeO-PCP being the 19th most used substance. There were 19 reports of 3-MeO-PCP use, compared with 110 for methoxetamine, the most popular substance. The drug was described positively, with users indicating it was relatively low risk for “addictiveness,” while it ranked high for people’s appreciation of the effects and their likelihood of using it again.
From October 2015 to October 2016, Wadsworth et al. (2018) collected data from 22 darknet markets. Seven bimonthly snapshots from the markets found 808 vendors selling 256 unique NPS. Most NPS were available inconsistently and 21% appeared in only one snapshot. However, there were 61 NPS (24%) that appeared in every snapshot, including 3-MeO-PCP, suggesting it was relatively popular.
Machado et al. (2019) retrospectively reported the contents of seized drug-containing material, particularly NPS, that was analyzed between May 2008 and December 2017 in Minas Gerais, the second most populous state in Brazil. 3-MeO-PCP was first detected in March 2017 and it was infrequently encountered.
Section 6: Legal Status
Note: This information is from March 2021. Always check your local laws to verify the current legal status of 3-MeO-PCP.
Australia
Australia has broad drug analog laws at the federal and state level. Because PCP is a Schedule 9 substance federally and it is also controlled at the state level, 3-MeO-PCP is similarly prohibited.
Canada
Federally, PCP is a Schedule I drug, along with its “salts, derivatives and analogues.” This would be expected to include 3-MeO-PCP, making it illicit.
United Kingdom
Class B.
As with other arylcyclohexylamine dissociatives, it is covered by a broad ban on derivatives of 1-phenylcyclohexylamine and 2-phenylcyclohexanone.
United States
Unscheduled.
However, 3-MeO-PCP is a close derivative of the Schedule II drug PCP and may be covered by the Federal Analogue Act when the drug is intended for human consumption.
Section 7: Safety
7.1 Overview
At typical doses, 3-MeO-PCP can increase heart rate and blood pressure, but its primary risks are psychological. Because the drug can trigger mania, delusions, and psychosis, dangerous and reckless behavior may occur. Users have been hospitalized, arrested, and injured under the influence. While these problems are particularly notable with 3-MeO-PCP because of its energizing and manic properties and its high potency, users who take light to common doses and avoid multiday use should be at a relatively low risk.
7.2 Non-Fatal Case Reports
Stevenson and Tuddenham (2014) described a case in which a male in his twenties was charged with the attempted murder of his father for an incident involving the use of 3-MeO-PCP, the stimulant methylenedioxypyrovalerone (MDPV), and butane gas. He insufflated large amounts of 3-MeO-PCP and MDPV, which produced auditory, visual, and tactile hallucinations. He reported meeting spirits, traveling to different worlds, feeling people touch him, and believing he could shoot fireballs from his fingers.
Eventually he had the idea that his home could be a base for superheroes and for that base to be established, he needed to kill his father (Stevenson and Tuddenham, 2014). Immediately after hearing a voice say, “kill him,” the user repeatedly stabbed his father, who only survived because neighbors heard the attack and called for emergency medical services. The user was arrested while in a stuporous state in his bedroom.
This case was complicated by the user’s medical history, which included hearing voices during a period of regular butane gas intake and those voices continued after stopping his use (Stevenson and Tuddenham, 2014). He responded to treatment with risperidone but had stopped taking his medication by the time of the attack, and in the intervening period he continued experiencing some hallucinations and voices, which he recognized were associated with his drug use. The authors determined it was likely that the individual was “particularly vulnerable” to psychiatric effects from these drugs due to his past history of drug-induced psychosis and his persistent symptoms. He was sentenced to four years in prison for attempted murder.
Out of 1243 cases of suspected novel psychoactive substance (NPS) intoxication included in Sweden’s STRIDA project between July 2013 and March 2015, 3-MeO-PCP was detected in the serum and/or urine of 56, while 4-MeO-PCP was found in 11, and both drugs were present in eight cases (Backberg et al., 2015). The mean serum concentration of 3-MeO-PCP was 29 ng/mL (range: 1 – 242 ng/mL) and the mean urine concentration was 4,281 ng/mL (range: 2 – 52,759 ng/mL). Biological sampling occurred within two hours of admission in 62% of cases, based on the 50 (85%) cases for which the sampling time was known.
Most cases (n=55) involved additional drugs, while the rest (n=7) only involved 3-MeO-PCP (Backberg et al., 2015). Ethanol and cannabis were the most common coadministered drugs overall, while the most common NPS were 5-MeO-MiPT and 4F-PVP.
Among both single-substance and polydrug cases, hypertension (SBP ≥140 mmHg), altered mental status (e.g. confusion, disorientation, dissociation, and/or hallucinations), and tachycardia (HR ≥100 bpm) were the most common symptoms of 3- and 4-MeO-PCP exposure (Backberg et al., 2015). The symptoms in the seven cases where 3-MeO-PCP was the only drug detected included: agitation (n=2), nystagmus (n=2), renal deficiency (n=2), miosis (n=2), pupils that did not respond to light or responded slowly (n=1), rhabdomyolysis (n=1), and diaphoresis (n=1).
Treatment with benzodiazepines (mostly diazepam and/or midazolam) was reported in 44% of cases, while propofol was used in 22%, and haloperidol was used in 8% (Backberg et al., 2015). Hospitalization usually did not last long, with most patients (85%) leaving after 1-2 days, and the mean hospitalization duration was two days (range: 1-9 days). Observation and treatment in the ICU was deemed necessary in 47% of cases. Among the patients who only used 3-MeO-PCP, two were observed in the ICU and hospitalization never lasted beyond two days.
Two young males (19- and 21-years-old) were hospitalized while comatose and they presented with respiratory acidosis, anisocoria (unequal pupil size), mydriasis, and hypothermia (Bertol et al., 2017). After a seven-hour period of intubation with minimal sedation, they awoke in an altered state and the 19-year-old was delirious and euphoric. They reported having taken a large amount of alcohol and unknown pills.
Both patients had intoxicating levels of alcohol in their blood (2.0 g/L for the 19-year-old and 1.7 g/L for the 21-year-old), but not life-threatening amounts (Bertol et al., 2017). 3-MeO-PCP was the only other drug detected and quantified using liquid chromatography-tandem mass spectrometry (LC-MS/MS). The concentrations were: 350.0 and 6,109.2 ng/mL in blood and urine from the 19-year-old, respectively; 180.1 and 3,003.5 ng/mL in blood and urine from the 21-year-old, respectively.
Three cases of 3-MeO-PCP exposure were captured by the Colorado site of the Psychoactive Surveillance Consortium and Analysis Network (PSCAN), which analyses the clinical symptoms and biological samples from patients seeking medical care after NPS use (Brandehoff et al., 2018). Eight cases of reported “Black Mamba” use (a synthetic cannabinoid product associated with ADB-FUBINACA) were discussed in the paper. Three patients had 3-MeO-PCP in urine (but not serum), and only one of those patients (Case 3) had a synthetic cannabinoid in their system.
“Black Mamba” use was reported by all three patients, along with cocaine (Case 1), methamphetamine (Case 2), and ethanol (Case 3) (Brandehoff et al., 2018). Case 1 (42-year-old female) had a depressed mental status, combative behavior, a seizure, a max BP of 139/80 mmHg, and a max HR of 92 bpm—treatment involved diazepam, potassium, and levetiracetam. Case 2 (36-year-old female) had chest pain, agitation, a max BP of 199/118 mmHg, and a max HR of 147—treatment involved saline, diazepam, ketorolac, lisinopril, and hydrocodone. And Case 3 (29-year-old male) had agitation, CNS depression, a max BP of 120/70 mmHg, and a max HR of 93—no treatment was given.
All patients were discharged after observation in the emergency department, with lengths of stay of 26 hours (Case 1), 8 hours (Case 2), and 5 hours (Case 3) (Brandehoff et al., 2018). 3-MeO-PCP was detected in urine at the following concentrations: 114.1 ng/mL (Case 1), 60.3 ng/mL (Case 2), and 103.2 ng/mL (Case 3).
Johansson et al. (2017) published information from one non-fatal intoxication involving 3-MeO-PCP. Emergency medical services were called to assist a 19-year-old male who was depressed, suicidal, and exhibiting erratic behavior. His initial presentation included a respiratory rate of 22, HR 130 bpm, BP 147/104 mmHg, oxygen saturation 96%, and normal blood glucose (5.4 mmol/L). He was catatonic, had a Glasgow Coma Scale (GCS) score of 11, and his pupils were dilated but reactive to light.
At the hospital, the patient presented with tachypnea (rapid breathing), hypertension, catatonia, and mydriasis, which then worsened into fever, lactic acidosis, psychomotor agitation, and hallucinations (Johansson et al., 2017). He was hospitalized for 35 hours (2.5 hours in ED, 22 hours in ICU, then psychiatric ward).
3-MeO-PCP was the only drug identified in the patient’s blood, except for the medications provided during hospitalization (diazepam, haloperidol, propofol) (Johansson et al., 2017). Four blood samples were taken, providing insight into the drug’s kinetics. The concentrations in femoral blood were: 0.14 μg/g (admission to ED), 0.08 μg/g (2.5 hours post-admission), 0.06 μg/g (5 hours post-admission), and 0.04 μg/g (17 hours post-admission). Assuming typical first-order elimination kinetics, the half-life was estimated to be 11 hours.
Thornton et al. (2017) reported a case in which a 27-year-old male presented eight hours after insufflating a product that was obtained online, which caused strange and “distant” behavior that alarmed his family members. He had a history of bipolar disorder, ADHD, and hypertension. Initially his temperature was normal (37.0°C), HR was 114 bpm, BP was 185/116 mmHg, respiration rate was 19, and oxygen saturation was 98%. His speech was clear, but his affect was odd and his responses to questions were sometimes delayed by more than one minute. Other symptoms included occasional inappropriate laughter, inability to recall events of the past 8-12 hours (despite being relatively well-oriented), and staring off when he was not being questioned. No active visual or auditory hallucinations were reported.
The patient exhibited upward vertical nystagmus spontaneously and upon exam, his reflexes were normal, strength and sensation were grossly normal, and he could stand, but was unable to walk without assistance because of imbalance (Thornton et al., 2017). He reported having taken 20 mg of “MXE” and denied other drug use, aside from his normal prescriptions (lithium, methylphenidate, and trazodone). During eight hours of observation, his mental status normalized, BP reduced to 138/88 mmHg, and HR reduced to 75 bpm.
A urine immunoassay drug screen (EMIT II Plus) was positive for PCP and THC-COOH, but neither drug was detected in serum upon further analysis using LC-QTOF-MS (Thornton et al., 2017). Instead, MXE and 3-MeO-PCP were detected in three serum samples taken at admission, two hours post-admission, and three hours post-admission. The levels were:
- 3-MeO-PCP (ng/mL): 167 (0 h), 131 (2 h), and 90 (3 h).
- MXE (ng/mL): 279 (0 h), 205 (2 h), and 180 (3 h).
Eight drug products were brought in by the patient’s family for analysis (Thornton et al., 2017). One product labeled “1” contained 3-MeO-PCP and two others contained MXE.
Two males who consumed a powder and alcohol at a party reportedly experienced disorientation, hallucinations, spastic leg postures, and facial grimacing ~15 minutes after drug intake (Zidkova et al., 2017). During transport to the hospital they exhibited hypertension and received flumazenil and naloxone, neither of which had any effect.
Case 1 was a 37-year-old male who was admitted ~2 hours after drug intake, at which time he was hypertensive (170/100 mmHg), tachycardic (120 bpm), had prominent signs of psychosis, displayed an altered mental status with a GCS of 10-12, his muscle tone was increased, and he had spastic leg postures (Zidkova et al., 2017). Initially the patient did not respond to commands and was incomprehensibly shouting. Abnormal lab findings included: hypophosphatemia (0.55 mmol/L) and elevated arterial lactate (2.0 mmol/L). He received gastric lavage with multiple applications of activated charcoal, along with a gastrointestinal tract washout using macrogol (polyethylene glycol), metoclopramide, and neostigmine. Full consciousness returned in the following hours and he was cooperative with no hemodynamic or neurologic symptoms. The patient reported amnesia for the period of intoxication and was discharged after 24 hours in the ICU.
Case 2 was a 40-year-old male who had been referred to the ICU for cramps and a deteriorating state of consciousness (Zidkova et al., 2017). At admission, he was hypertensive (172/113 mmHg), tachycardic (126 bpm), breathing spontaneously, and normoglycemic. He had an altered state of consciousness (GCS: 12), maintained eye contact, did not obey commands, and had miotic pupils. Abnormal lab findings included: elevated arterial lactate (3.2 mmol/L), pH 7.289, and base deficit (6.0 mmol/L). Consciousness was fully regained over the following three hours and the patient was alert, cooperative, and showed hemodynamic improvement (BP 154/85 mmHg; HR 85). He had amnesia for the duration of the episode and was discharged eight hours after admission.
Although a positive result for PCP was found on urine immunoassays in both patients, 3-MeO-PCP was identified by LC-HRMS in serum and urine (Zidkova et al., 2017). Two hours after drug intake, the serum levels were 49 ng/mL (Case 1) and 66 ng/mL (Case 2). Other drugs were likely important in both cases. Case 1 had an intoxicating level of ethanol (102 mg/dL), while Case 2 had a normal methamphetamine serum level (0.121 mg/L) with amphetamine as a metabolite (0.01 mg/L).
Chang and Smith (2017) reported a case in which a 27-year-old male with a history of schizophrenia and ongoing auditory hallucinations due to noncompliance with risperidone therapy was found unconscious in his car by police. At the hospital he was awake, partially oriented, and followed simple commands. He also felt sedated and “loopy,” lacked any memory of the period before hospitalization, and described experiencing delusions (e.g. that he was an “alien with green blood”). Borderline tachycardia was the only abnormal vital sign. Notable lab results included: hypokalemia (potassium: 3.1 mmol/L), hypophosphatemia (phosphorus: 0.7 mg/dL), elevated AST (60 U/L), and indirect bilirubinemia (3.7 mg/dL). The first troponin I level was elevated (0.16 ng/mL) and it peaked five hours later at 0.21 ng/mL, suggestive of myocardial damage. Elevated CK was also noted (1017 U/L). He was medically stable by the second day in the hospital and at the time of discharge, his CK had decreased to 403 U/L.
At admission, the urine immunoassay only gave a positive result for PCP, but confirmatory testing with GC-MS revealed 3-MeO-PCP was present instead (Chang and Smith, 2017). No other drugs were detected. While the patient’s schizophrenia may have contributed to the symptoms, the authors believed the significant confusion and amnesia was more attributable to 3-MeO-PCP use.
A 17-year-old male was admitted to the ED because of altered consciousness and agitation, and he alternated between hypotonia and hypertonia (Allard et al., 2019). He had a bag of white powder labeled “3-MeO-PCP” in his belongings. His pupils were partly dilated and reactive to light. The patient was transferred to the ICU with rhabdomyolysis and slightly elevated serum CK, then he was discharged on Day 2. Analysis of his blood and urine revealed the presence of 3-MeO-PCP and 12 metabolites (seven phase I, five phase II). Metabolism involved hydroxylation of the piperidine and/or cyclohexyl rings, as well as O-demethylation.
3-MeO-PCP was identified in a 39-year-old female who was found dead in her home due to an assault by her partner in which he strangled her while under the influence of multiple drugs, but not 3-MeO-PCP (Kintz et al., 2019). Analysis with GC-MS identified 3-MeO-PCP in the victim’s femoral blood at a concentration of 63 ng/mL. She also had an intoxicating blood alcohol concentration (137 mg/dL) and other drugs were present in blood: diazepam (157 ng/mL) and its metabolite nordiazepam (204 ng/mL), and cocaine (25 ng/mL) and its metabolites benzoylecgonine (544 ng/mL) and cocaethylene (43 ng/mL).
In addition to blood, 3-MeO-PCP was quantified in bile (64 ng/mL), urine (94 ng/mL), and in three hair segments: 731 pg/mg (0-2 cm), 893 pg/mg (2-4 cm), and 846 pg/mg (4-6 cm) (Kintz et al., 2019). The hair results were indicative of 3-MeO-PCP use spanning a period of months. The authors determined that the victim’s reported symptoms before death, i.e. visual hallucinations and behavioral alteration, were attributable to 3-MeO-PCP and the influence of the other CNS depressants taken by the victim.
Berar et al. (2019) reported a case of a 17-year-old male accidentally taking 200 mg 3-MeO-PCP orally, an excessively high dose, and although he experienced hemodynamic, psychological, and neurological symptoms, he survived. He was initially admitted to the ED for agitation and consciousness disorders, and he alternated between hypotonia and hypertonia, alongside mental fog, agitation, and limb tremor. The patient was hypertensive (158/131 mmHg), tachycardic (100 bpm), and had a normal oxygen saturation of 99%. His respiration was not impaired, and an ECG was unremarkable. He developed nystagmus and dysarthria (slurred speech), and his deep tendon reflexes were brisk.
Lab findings included hyperlactatemia (2.6 mmol/L) and elevated serum CK (290 U/L) (Berar et al., 2019). There was no evidence of liver or kidney failure. He received midazolam (1 mg) for hypertonia, and he was also treated with saline infusion. After he was transferred to the ICU, serum CK increased (339 U/L) but his lactate normalized. To manage agitation, sedative antipsychotics (cyamemazine and loxapine) were given. Within 24 hours, the neurological symptoms were alleviated, and his BP and HR normalized. Mild sedation continued but was withdrawn the next day. Blood and urine analysis confirmed he had taken 3-MeO-PCP, and quantification using LC-HRMS a few hours after drug intake showed 71.1 ng/mL in peripheral blood and 706.9 ng/mL in urine. The patient said he took 200 mg because he accidentally followed the dosing information for 4-MeO-PCP, which is much less potent.
One week after the first incident, the same patient was admitted to the ED after insufflating 50 mg 3-MeO-PCP (Berar et al., 2019). Again, his BP (150/104 mmHg) and HR (105 bpm) were elevated, while oxygen saturation (96%) was normal. He displayed slight psychomotor impairment and dysarthria, but his neurological examination was essentially normal, including an absence of consciousness disorders, limb tremor, and hypertonia. He was discharged after 12 hours of monitoring.
Three cases of 3-MeO-PCP use were detected during a one-week period in a single town in France (Grossenbacher et al., 2019). Case 1 was a 36-year-old male who was found agitated on the street while crying that PCP was the best drug in the world. Once he was in the ED, the patient exhibited at different times confusion, aggressiveness, logorrhea (speech that is excessive, rapid, and pressured), hypertonia, miosis, hypersalivation, and eventually calmness. He was hypertensive (151/90 mmHg), tachycardic (100 bpm), normoglycemic (5 mmol/L), and normothermic (37.3°C). Elevated CK (273 U/L) was present, but his liver enzymes and creatinine were normal. Alcohol was present, urine testing was positive for buprenorphine, and GC-MS identified 3-MeO-PCP. He received midazolam (5 mg) and the symptoms lasted for six hours.
In Case 2, a 32-year-old male with a history of significant cannabis use presented to the ED for abdominal pains (Grossenbacher et al., 2019). Analgesics (morphine, paracetamol, and nefopam) were ineffective. BP (137/87 mmHg) and glucose (8.1 mmol/L) were somewhat elevated, while HR (83 bpm) and temperature (36°C) were normal. Urine drug screening was positive for opiates and THC-COOH, and 3-MeO-PCP was identified qualitatively. Cannabis hyperemesis was the suspected cause of the patient’s condition.
Lastly, Case 3 involved a routine urine drug test on a methadone user who was not experiencing any clinical symptoms but had trace amounts of 3-MeO-PCP as shown by GC-MS (Grossenbacher et al., 2019).
Minutes after reportedly taking 0.2 mg 3-MeO-PCP intravenously, a 40-year-old male was found unconscious while lying on the ground by his partner (van den Bersselaar et al., 2021). Because his decreased consciousness remained six hours later and the patient was exhibiting strange behavior and appeared anxious, his partner called for emergency medical services. His vitals were not severely altered, with a respiratory rate of 18 breaths per minute, oxygen saturation 96%, normal peripheral pulse, and sinus tachycardia of 115 bpm. Decreased consciousness with a GCS of 8 (E2M5V1) was reported by ambulance staff, but that improved to a GCS of 12 (E3M5V4) in the ED.
The patient constantly moved his extremities, but without rigidity, spasms, or clonus—this extreme motor activity prevented BP measurement (van den Bersselaar et al., 2021). He was very anxious, believed he was dead, and kept grasping his extremities while staring at them as though they were not his. The medical staff could not draw his attention or communicate with him, and the patient appeared unaware of his surroundings. Some lab tests were abnormal: elevated CK (1501 U/L), elevated troponin T (20 ng/L), and low potassium (3.4 mmol/L). His ECG was normal.
According to the patient, he had taken 3-MeO-PCP for the first time on the day of the ED admission (van den Bersselaar et al., 2021). The effects were more intense than his typical drug of choice, 4P (4-methylethcathinone/pentedrone), and he did not remember anything after injecting the drug. A sample of the product he used showed it contained 3-MeO-PCP and a byproduct, piperidine cyclohexane carbonitrile (PCC).
7.3 Fatalities
A 29-year-old male insufflated “fumaric acid” and was later found unresponsive in his bed, resuscitation efforts failed, and he was pronounced dead shortly after arriving at the hospital (Bakota et al., 2016). An ELISA screen of postmortem blood indicated the presence of PCP, amphetamine, and a cannabis metabolite. Diphenhydramine (DPH) was also detected with further screening techniques. Analysis with LC-TOFMS detected 3-MeO-PCP, not PCP.
The postmortem blood concentration of 3-MeO-PCP was 139 ng/mL (Bakota et al., 2016). Testing also confirmed DPH in blood and stomach contents. DPH was found at a supratherapeutic concentration (4,100 ng/mL) and was considered likely to have contributed to the death. A relatively small amount of amphetamine (<0.10 mg/L) was present in blood. Because the physiologic effects (e.g. cardiovascular effects) of 3-MeO-PCP, DPH, and amphetamine are similar, the combined effects of all three drugs were considered the cause of death. A bag of white powder labeled “fumaric acid 5 G” was found next to the decedent but its contents were not tested. However, based on the toxicological findings, fumaric acid was not responsible for the death.
Seven fatalities in Sweden between March 2014 and June 2016 were discussed by Johansson et al. (2017). Details from those cases are as follows (all drug concentrations are from femoral blood):
- Case 1: 27-year-old male found dead in their bathtub at home. Autopsy showed cerebral edema and pulmonary edema.
- Toxicology (μg/g)
- 3-MeO-PCP: 0.38
- No other drugs found.
- Cause of death: Intoxication with 3-MeO-PCP.
- Toxicology (μg/g)
- Case 2: 21-year-old suicidal male found unresponsive in bed after snoring loudly through the night. After an hour of cardiopulmonary resuscitation, he was pronounced dead. Autopsy showed cerebral edema, pulmonary edema, patent foramen ovale (a hole in the heart, which is common, occurring in 25% of people), and discrete coronary atherosclerosis. He reportedly used alcohol, buprenorphine, and possibly other drugs.
- Toxicology (μg/g)
- 3-MeO-PCP: 0.18
- Other drugs: buprenorphine (2.2), norbuprenorphine (1.1), 5-MeO-MiPT (0.13).
- Cause of death: Intoxication with buprenorphine, 3-MeO-PCP, and 5-MeO-MiPT.
- Toxicology (μg/g)
- Case 3: 27-year-old male found dead in his apartment. Autopsy showed congestion of the liver and lungs.
- Toxicology (μg/g)
- 3-MeO-PCP: 0.23
- Other drugs: methadone (0.44), diazepam (0.53), nordazepam (0.62), temazepam (0.03), oxazepam (0.04), pregabalin (2.7), methamphetamine (0.04), buprenorphine (0.2), norbuprenorphine (0.7).
- Cause of death: Mixed drug intoxication.
- Toxicology (μg/g)
- Case 4: 29-year-old male found hanged in his apartment. He had a history of bipolar disorder and had written a suicide note. Autopsy showed cerebral edema, pulmonary congestion and edema, discrete coronary atherosclerosis, enlarged liver, and petechial hemorrhage of the oral mucosa.
- Toxicology (μg/g)
- 3-MeO-PCP: 0.12
- Other drugs: nordazepam (0.09), pregabalin (14), flubromazolam (0.01), AB-FUBINACA, THJ-018, buprenorphine (2.0), norbuprenorphine (2.3), methylphenidate (0.02), ritalinic acid (0.48).
- Cause of death: Asphyxia.
- Toxicology (μg/g)
- Case 5: 32-year-old male found dead in his apartment. Autopsy revealed fresh myocardial injury, congestion of internal organs, edema of lungs, brain, and heart. There were signs of incipient pneumonia and aspiration of stomach contents.
- Toxicology (μg/g)
- 3-MeO-PCP: 0.06
- Other drugs: oxycodone (0.10), amphetamine (0.13), flubromazolam (0.009), MT-45 (0.11), 4-MeO-PCP (0.03), THJ-018, THC (0.0011).
- Cause of death: Mixed drug intoxication.
- Toxicology (μg/g)
- Case 6: 27-year-old male found unresponsive in bed after snoring early in the morning. He was pronounced dead at the scene following unsuccessful resuscitation attempts. Autopsy showed congestion of internal organs, pulmonary edema, and petechiae on the surface of the heart.
- Toxicology (μg/g)
- 3-MeO-PCP: 0.05
- Other drugs: tramadol (0.06), alprazolam (0.02), fentanyl (25), amphetamine (0.09).
- Cause of death: Intoxication with fentanyl.
- Toxicology (μg/g)
- Case 7: 20-year-old female found dead in bed. She reportedly took tramadol and benzodiazepines the night before. Autopsy showed pulmonary and cerebral edema, and congestion of internal organs.
- Toxicology (μg/g)
- 3-MeO-PCP: 0.08
- Other drugs: tramadol (13), O-desmethyltramadol (4.9)
- Cause of death: intoxication with tramadol and O-desmethyltramadol.
- Toxicology (μg/g)
The fatalities were caused by intoxication in six cases, while asphyxia was the cause in Case 4 (Johansson et al., 2017). 3-MeO-PCP was only considered the cause of death in Case 1, which also involved the largest 3-MeO-PCP concentration (0.38 μg/g; ~380 ng/mL), and it was listed as a contributing factor in Cases 2, 3, and 5. The femoral blood concentrations were 0.05 to 0.38 μg/g, which is roughly 50 to 380 ng/mL, similar to the concentrations reported in other 3-MeO-PCP cases.
Mitchell-Mata et al. (2017) reported two deaths in Washington State that involved larger 3-MeO-PCP concentrations than most cases. Case 1 was a 21-year-old male with a history of drug use who was found naked and unresponsive in a pigsty. Case 2 was a 58-year-old male with a history of drug use who was found unresponsive in a “clean and sober” house.
In Case 1, ethanol was detected at an intoxicating level of 0.047 g/dL, and Case 2 had a presumptive positive result for PCP in blood as detected by enzyme multiplied immunoassay technique (EMIT) as well as a presumptive positive for amphetamines in urine (Mitchell-Mata et al., 2017). Analysis with GC-MS showed Case 1 was positive for 3-MeO-PCP, bupropion, delorazepam, mitragynine, and paroxetine, while Case 2 was positive for 3-MeO-PCP and methamphetamine. The 3-MeO-PCP concentrations in blood were 3,200 ng/mL in Case 1 and 630 ng/mL in Case 2.
The first reported fatality linked to 3-MeO-PCP in the Netherlands was a male in his mid-thirties who was found dead at the edge of a lake (de Jong et al., 2019). His medical history indicated substance use disorder, specifically with amphetamine and THC. The decedent and a friend used an “ant poison” named “Thrive Soluble” the night before, and the effect of this “ant poison” was that they lost control of their behavior. “Thrive Soluble” is not an ant poison in the Netherlands, but rather a product sold online as “not for human use,” suggesting it is an NPS.
A bag of the “ant poison” was provided to the police by the decedent’s friend and it was shown to be 3-MeO-PCP, which was also present in blood and serum (de Jong et al., 2019). The serum level was 123 ng/mL and the blood level was 152 ng/mL. The only other drug detected in serum was amphetamine at a common concentration (85 ng/mL), and ethanol was present in blood. The cause of death was mixed drug intoxication with 3-MeO-PCP, amphetamine, and alcohol.
Without specifying the isomer, “MeO-PCP” was identified in a 31-year-old male who was found vomiting and convulsing, resulting in a call for emergency medical services (Krotulski et al., 2018). The revival attempt, including the use of naloxone, was unsuccessful and he was pronounced dead at the scene. The autopsy findings were consistent with opioid overdose, including pulmonary congestion and edema, and mild cerebral edema.
Urine immunoassay gave presumptive positive results for benzodiazepines, PCP, and fentanyl (Krotulski et al., 2018). Analysis of urine and blood via LC-MS/MS found there were quantifiable levels of tetrahydrofuranylfentanyl (THFF), U-49900, and MeO-PCP. In blood, the levels were: THFF (339 ng/mL), U-49900 (1.5 ng/mL), and MeO-PCP (1.0 ng/mL). In urine, the levels were: THFF (>5,000 ng/mL), U-49900 (2.2 ng/mL), and MeO-PCP (31.8 ng/mL). Additionally, a range of other drugs were present in blood: naloxone, alprazolam (10 ng/mL), paroxetine (10 ng/mL), topiramate (6,500 ng/mL), zolpidem (8.6 ng/mL), trazodone (360 ng/mL), aripiprazole (170 ng/mL), chlorpheniramine (63 ng/mL), dextro/levomethorphan (46 ng/mL) and promethazine (27 ng/mL).
The death was attributed to accidental acute intoxication with THFF, U-49900, and MeO-PCP (Krotulski et al., 2018). MeO-PCP was likely 3- or 4-MeO-PCP, and 3-MeO-PCP could be more likely as it appears to be a more popular drug. Regardless, MeO-PCP may not have been a major factor in the fatality considering the blood concentration was far lower than has been reported in other cases of intoxication or death.
7.4 Tolerance and Withdrawal (Physical Dependence)
Tolerance
Tolerance builds quickly and it often lasts longer than with other drug classes, particularly with heavy use. At light to common doses, it may provide largely similar effects for a number of days and perhaps longer if the user is looking for non-dissociative effects (e.g. energy, mood enhancement, motivation, anxiolysis). The full dissociative effects associated with common to strong doses become progressively harder to attain within a few days of use.
With substantial use, such as daily use of low to common doses or higher doses taken weekly for weeks or months, some degree of tolerance may last weeks to months after complete cessation, according to subjective reports.
After effects / withdrawal
After an extended period of use, the perceived benefits (e.g. mood enhancement, increased motivation) can flip around for days to weeks after cessation. Users may experience low mood, anhedonia, a persistent sense of disconnection from their body and environment, and low motivation.
Either because of real impairment induced by toxicity or as a byproduct of dissociation, lack of interest, and low mood, people can feel cognitively impaired, often with memory impairment and difficulty coming up with the desired word to use in conversation.
Withdrawal is minimal to nonexistent if the drug is taken for less than a few days. That pattern of use is normally associated with little more than subjective cognitive impairment and a hangover feeling for a couple of days.
7.5 Drug Interactions
Warning
This section covers some, not all, potential drug interactions. Because there are countless substances that it could interact with and 3-MeO-PCP has been minimally researched, there is no way to list and describe every interaction. In general, it is best to avoid mixing this substance with other drugs.
Benzodiazepines
Benzodiazepines are sometimes used to counter the negative effects of 3-MeO-PCP and other dissociatives, such as anxiety, insomnia, and restlessness. While this can help in some cases, it is not recommended, particularly when common to strong doses of 3-MeO-PCP have been used. Benzodiazepines can exacerbate disinhibition, confusion, cognitive impairment, and physical impairment. This increases the likelihood of poor decision-making and accidental injury.
Both 3-MeO-PCP and benzodiazepines also come with potential redosing issues. In addition to the risk of compulsive redosing, the cognitive impairment associated with these drugs could interfere with one’s memory of how much benzodiazepine (or 3-MeO-PCP) they have already taken and how long it has been since either drug was used. As such, a user could easily find themselves taking excessive benzodiazepine doses because they have not waited long enough for the effects to begin or because they have already forgotten that they took a benzodiazepine earlier.
Taking light to common doses of 3-MeO-PCP in the presence of a trusted, sober friend is usually a better strategy for reducing anxiety, paranoia, and bad decision-making. If a user loses control of their behavior and is at risk of accidentally harming themselves or others, they can be better treated in a medical setting, where benzodiazepines and other sedatives are safer to administer.
Cannabis
Cannabis is frequently combined with 3-MeO-PCP, and while this can be a good combination at the right dose of both substances, a lot of caution is warranted. Even a small amount of cannabis can greatly increase the effects, which may be a problem, especially in those who are not long-term cannabis users.
Among the potential effects are increased open-eye visuals (OEVs) and closed-eye visuals (CEVs), music enhancement, introspection, and elevated mood. However, it also comes with a significant potential to trigger anxiety and paranoia, along with more psychotic, manic, and delusional effects.
The best general recommendation is to avoid this combination. Those who still decide to try it should already be highly experienced with cannabis and they should begin with very small amounts. Preferably it will only be combined with light to common doses of 3-MeO-PCP, if used at all.
Alcohol
Some users enjoy the effects of low doses combined with up to a few drinks, including in social settings where the effects can be additive or synergistic. This is risky, however. Although the effects can be safe and pleasant when the right doses are used, most of the concerns outlined for benzodiazepines also apply to alcohol. The adverse effects can include impaired decision-making, physical impairment, and memory loss.
Alcohol may pose a greater risk than benzodiazepines because of its tendency to cause vomiting, particularly at high doses. If someone is highly impaired or unconscious, vomit may block their airway and/or reach their lungs, causing potentially fatal aspiration pneumonia.
This combination is best avoided. If it is still taken, both drugs should not go beyond their respective light to common doses.
Other substances
These are some of the drugs that may be dangerous to combine with 3-MeO-PCP:
GHB (and GBL, BDO)
Some of the potential risks are deep unconsciousness, impaired decision-making, vomit aspiration, cognitive impairment, respiratory depression, and physical impairment (e.g. difficulty moving safely).
Tramadol
Tramadol has at least two major components of its pharmacology that require it to be treated like an opioid and an SNRI (serotonin-norepinephrine reuptake inhibitor). Therefore, it comes with opioid-type risks (e.g. respiratory depression, unconsciousness, physical and cognitive impairment, vomit aspiration) and a higher risk of seizures.
Opioids
Some of the potential risks are deep unconsciousness, vomit aspiration, cognitive impairment, respiratory depression, and physical impairment.
Amphetamines
There may be an additive cardiovascular effect, as both amphetamines and 3-MeO-PCP can increase heart rate and blood pressure. Additionally, amphetamines could significantly increase the risk of mania, psychosis, and delusions.
Cocaine
There may be an additive cardiovascular effect, as both cocaine and 3-MeO-PCP can increase heart rate and blood pressure. Additionally, cocaine could significantly increase the risk of mania, psychosis, and delusions.
Section 8: References
Allard, S., Allard, P., Morel, I., & Gicquel, T. (2019). Application of a molecular networking approach for clinical and forensic toxicology exemplified in three cases involving 3‐MeO‐PCP, doxylamine, and chlormequat. Drug Testing and Analysis, 11(5), 669–677. https://doi.org/10.1002/dta.2550
Ameline, A., Greney, H., Monassier, L., Raul, J., & Kintz, P. (2019). Metabolites to parent 3-MeO-PCP ratio in human urine collected in two fatal cases. Journal of Analytical Toxicology, 43(4), 321–324. https://doi.org/10.1093/jat/bky097
Åstrand, A., Guerrieri, D., Vikingsson, S., Kronstrand, R., & Green, H. (2020). In vitro characterization of new psychoactive substances at the μ-opioid, CB1, 5HT1A, and 5-HT2A receptors—On-target receptor potency and efficacy, and off-target effects. Forensic Science International, 317, 110553. https://doi.org/10.1016/j.forsciint.2020.110553
Bäckberg, M., Beck, O., & Helander, A. (2015). Phencyclidine analog use in Sweden—Intoxication cases involving 3-MeO-PCP and 4-MeO-PCP from the STRIDA project. Clinical Toxicology, 53(9), 856–864. https://doi.org/10.3109/15563650.2015.1079325
Bäckberg, M., Jönsson, K.-H., Beck, O., & Helander, A. (2018). Investigation of drug products received for analysis in the Swedish STRIDA project on new psychoactive substances. Drug Testing and Analysis, 10(2), 340–349. https://doi.org/10.1002/dta.2226
Bakota, E., Arndt, C., Romoser, A. A., & Wilson, S. K. (2016). Fatal Intoxication Involving 3-MeO-PCP: A Case Report and Validated Method. Journal of Analytical Toxicology, 40(7), 504–510. https://doi.org/10.1093/jat/bkw056
Beagle, J. Q. (n.d.). Synthesis and Effects of PCP Analogs. Retrieved March 5, 2021, from https://www.erowid.org/archive/rhodium/chemistry/pcp/sar.html#saramine
Berar, A., Allain, J.-S., Allard, S., Lefevre, C., Baert, A., Morel, I., Bouvet, R., & Gicquel, T. (2019). Intoxication with 3-MeO-PCP alone: A case report and literature review. Medicine, 98(52), e18295. https://doi.org/10.1097/MD.0000000000018295
Bertol, E., Pascali, J., Palumbo, D., Catalani, V., Di Milia, M. G., Fioravanti, A., Mari, F., & Vaiano, F. (2017). 3-MeO-PCP intoxication in two young men: First in vivo detection in Italy. Forensic Science International, 274, 7–12. https://doi.org/10.1016/j.forsciint.2016.12.028
Bluelight. (2009). 1-{1-(3-Methoxiphenyl)-cyclohexyl}-piperidin. https://www.bluelight.org/xf/threads/1-1-3-methoxiphenyl-cyclohexyl-piperidin.427958/
Brandehoff, N., Adams, A., McDaniel, K., Banister, S. D., Gerona, R., & Monte, A. A. (2018). Synthetic cannabinoid “Black Mamba” infidelity in patients presenting for emergency stabilization in Colorado: A P SCAN Cohort. Clinical Toxicology, 56(3), 193–198. https://doi.org/10.1080/15563650.2017.1357826
Chang, B. N., & Smith, M. P. (2017). A Case of Unusual Drug Screening Results. Clinical Chemistry, 63(5), 958–961. https://doi.org/10.1373/clinchem.2016.264507
de Jong, L. A. A., Olyslager, E. J. H., & Duijst, W. L. J. M. (2019). The risk of emerging new psychoactive substances: The first fatal 3-MeO-PCP intoxication in The Netherlands. Journal of Forensic and Legal Medicine, 65, 101–104. https://doi.org/10.1016/j.jflm.2019.05.011
EMCDDA-Europol. (2013). New drugs in Europe, 2012. EMCDDA–Europol 2012 Annual Report on the implementation of Council Decision 2005/387/JHA. https://www.emcdda.europa.eu/system/files/publications/734/EMCDDA-Europol_2012_Annual_Report_final_439477.pdf
EMCDDA-Europol. (2015). EMCDDA–Europol 2014 Annual Report on the implementation of Council Decision 2005/387/JHA. https://www.emcdda.europa.eu/system/files/publications/1018/TDAN15001ENN.pdf
Grossenbacher, F., Cazaubon, Y., Feliu, C., Ameline, A., Kintz, P., Passouant, O., Mourvillier, B., & Djerada, Z. (2019). About 5 cases with 3 Meo-PCP including 2 deaths and 3 non-fatal cases seen in France in 2018. Toxicologie Analytique et Clinique, 31(4), 332–336. https://doi.org/10.1016/j.toxac.2019.10.004
Helander, A., Bäckberg, M., & Beck, O. (2020). Drug trends and harm related to new psychoactive substances (NPS) in Sweden from 2010 to 2016: Experiences from the STRIDA project. PLOS ONE, 15(4), e0232038. https://doi.org/10.1371/journal.pone.0232038
Johansson, A., Lindstedt, D., Roman, M., Thelander, G., Nielsen, E. I., Lennborn, U., Sandler, H., Rubertsson, S., Ahlner, J., Kronstrand, R., & Kugelberg, F. C. (2017). A non-fatal intoxication and seven deaths involving the dissociative drug 3-MeO-PCP. Forensic Science International, 275, 76–82. https://doi.org/10.1016/j.forsciint.2017.02.034
Kintz, P., Ameline, A., Walch, A., Farrugia, A., & Raul, J.-S. (2019). Murdered while under the influence of 3-MeO-PCP. International Journal of Legal Medicine, 133(2), 475–478. https://doi.org/10.1007/s00414-018-1901-x
Krotulski, A. J., Papsun, D. M., Friscia, M., Swartz, J. L., Holsey, B. D., & Logan, B. K. (2018). Fatality Following Ingestion of Tetrahydrofuranylfentanyl, U-49900 and Methoxy-Phencyclidine. Journal of Analytical Toxicology, 42(3), e27–e32. https://doi.org/10.1093/jat/bkx092
Machado, Y., Coelho Neto, J., Lordeiro, R. A., Silva, M. F., & Piccin, E. (2019). Profile of new psychoactive substances (NPS) and other synthetic drugs in seized materials analysed in a Brazilian forensic laboratory. Forensic Toxicology, 37(1), 265–271. https://doi.org/10.1007/s11419-018-0456-3
Maddox, V. H., Godefroi, E. F., & Parcell, R. F. (1965). The Synthesis of Phencyclidine and Other 1-Arylcyclohexylamines. Journal of Medicinal Chemistry, 8(2), 230–235. https://doi.org/10.1021/jm00326a019
Michely, J. A., Manier, S. K., Caspar, A. T., Brandt, S. D., Wallach, J., & Maurer, H. H. (2017). New Psychoactive Substances 3-Methoxyphencyclidine (3-MeO-PCP) and 3-Methoxyrolicyclidine (3-MeO-PCPy): Metabolic Fate Elucidated with Rat Urine and Human Liver Preparations and their Detectability in Urine by GC-MS, “LC-(High Resolution)-MSn” and “LC-(High Resolution)-MS/MS.” Current Neuropharmacology, 15(5). https://doi.org/10.2174/1570159X14666161018151716
Mitchell-Mata, C., Thomas, B., Peterson, B., & Couper, F. (2017). Two Fatal Intoxications Involving 3-Methoxyphencyclidine. Journal of Analytical Toxicology, 41(6), 503–507. https://doi.org/10.1093/jat/bkx048
Mitsuoka, T., Hanamura, K., Koganezawa, N., Kikura-Hanajiri, R., Sekino, Y., & Shirao, T. (2019). Assessment of NMDA receptor inhibition of phencyclidine analogues using a high-throughput drebrin immunocytochemical assay. Journal of Pharmacological and Toxicological Methods, 99, 106583. https://doi.org/10.1016/j.vascn.2019.106583
Morris, H., & Wallach, J. (2014). From PCP to MXE: A comprehensive review of the non-medical use of dissociative drugs: PCP to MXE. Drug Testing and Analysis, 6(7–8), 614–632. https://doi.org/10.1002/dta.1620
Rhumorbarbe, D., Morelato, M., Staehli, L., Roux, C., Jaquet-Chiffelle, D.-O., Rossy, Q., & Esseiva, P. (2019). Monitoring new psychoactive substances: Exploring the contribution of an online discussion forum. International Journal of Drug Policy, 73, 273–280. https://doi.org/10.1016/j.drugpo.2019.03.025
Roth, B. L., Gibbons, S., Arunotayanun, W., Huang, X.-P., Setola, V., Treble, R., & Iversen, L. (2013). The Ketamine Analogue Methoxetamine and 3- and 4-Methoxy Analogues of Phencyclidine Are High Affinity and Selective Ligands for the Glutamate NMDA Receptor. PLoS ONE, 8(3), e59334. https://doi.org/10.1371/journal.pone.0059334
Roth, B. L., Gibbons, S., Arunotayanun, W., Huang, X.-P., Setola, V., Treble, R., & Iversen, L. (2018). Correction: The Ketamine Analogue Methoxetamine and 3- and 4-Methoxy Analogues of Phencyclidine Are High Affinity and Selective Ligands for the Glutamate NMDA Receptor. PLOS ONE, 13(3), e0194984. https://doi.org/10.1371/journal.pone.0194984
Soussan, C., & Kjellgren, A. (2016). The users of Novel Psychoactive Substances: Online survey about their characteristics, attitudes and motivations. International Journal of Drug Policy, 32, 77–84. https://doi.org/10.1016/j.drugpo.2016.03.007
Stevenson, R., & Tuddenham, L. (2014). Novel psychoactive substance intoxication resulting in attempted murder. Journal of Forensic and Legal Medicine, 25, 60–61. https://doi.org/10.1016/j.jflm.2014.04.007
Thornton, S., Lisbon, D., Lin, T., & Gerona, R. (2017). Beyond Ketamine and Phencyclidine: Analytically Confirmed Use of Multiple Novel Arylcyclohexylamines. Journal of Psychoactive Drugs, 49(4), 289–293. https://doi.org/10.1080/02791072.2017.1333660
van den Bersselaar, L. R., van der Hoeven, J. G., & de Jong, B. (2021). Feeling Death, Being Alive: 4-Methylethcathinone/Pentedrone Addiction and 3-Methoxyphencyclidine Intoxication. Addictive Disorders & Their Treatment, 20(1), 69–73. https://doi.org/10.1097/ADT.0000000000000214
Vignon, J., Vincent, J.-P., Bidard, J.-N., Kamenka, J.-M., Geneste, P., Monier, S., & Lazdunski, M. (1982). Biochemical properties of the brain phencyclidine receptor. European Journal of Pharmacology, 81(4), 531–542. https://doi.org/10.1016/0014-2999(82)90342-9
Wadsworth, E., Drummond, C., & Deluca, P. (2018). The Dynamic Environment of Crypto Markets: The Lifespan of New Psychoactive Substances (NPS) and Vendors Selling NPS. Brain Sciences, 8(3), 46. https://doi.org/10.3390/brainsci8030046
Wallach, J., & Brandt, S. D. (2018). Phencyclidine-Based New Psychoactive Substances. In H. H. Maurer & S. D. Brandt (Eds.), New Psychoactive Substances (Vol. 252, pp. 261–303). Springer International Publishing. https://doi.org/10.1007/164_2018_124
Zidkova, M., Hlozek, T., Balik, M., Kopecky, O., Tesinsky, P., Svanda, J., & Balikova, M. A. (2017). Two Cases of Non-fatal Intoxication with a Novel Street Hallucinogen: 3-Methoxy-Phencyclidine. Journal of Analytical Toxicology, 41(4), 350–354. https://doi.org/10.1093/jat/bkx009