Sertraline is an antidepressant in the SSRI class. It’s used for depression, anxiety, panic disorder, OCD, and a number of other conditions.
After entering the market in the early 1990s, sertraline became one of the most popular antidepressants.
The drug is used in adults, adolescents, and children. There might be greater concerns and lower efficacy in young people.
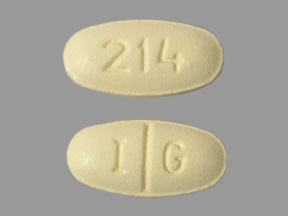
Sertraline = Zoloft; Lustral
PubChem: 68617
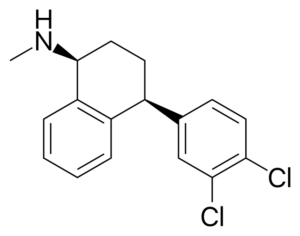
Molecular formula: C17H17Cl2N
Molecular weight: 306.23 g/mol
IUPAC: (1S,4S)-4-(3,4-dichlorophenyl)-N-methyl-1,2,3,4-tetrahydronaphthalen-1-amine
Contents
Dose
Oral
Initial: 25 – 50 mg/d
Maintenance: Typically 50 – 200 mg/d
The maintenance dose is determined by treatment response.
Timeline
Oral
Sertraline is usually taken once per day due to its long duration of action.
Experience Reports
Effects
Positive
- Anxiety reduction
- Mood improvement
- Depression reduction
Negative
- Nausea
- Headache
- Diarrhea
- Sexual dysfunction
- Insomnia
- Dry mouth
- Drowsiness
- Dizziness
- Tremor
- Fatigue
Efficacy has been demonstrated in depression, dysthymia, OCD, social anxiety, panic disorder, PTSD, premature ejaculation, and premenstrual dysphoric disorder. It’s also sometimes used for eating disorders.
The core effect of the substance is that it alters mood. This could mean less anxiety, less depression, a more positive outlook, improved cooperation with others, and greater assertiveness.
SSRIs may initially worsen symptoms like depression and anxiety in some people. This changes over a period of weeks, with the efficacy building over time.
Some benefits in depression may be noticed in the first 1-2 weeks, but the greatest clinical efficacy arrives in the first couple months.
Medical
Depression
Most of the evidence points to sertraline being more effective than placebo, with similar efficacy to other SSRIs, SNRIs, and TCAs.
Some trends in favor of it vs. other antidepressants may exist, making it a possible first-line treatment. It’s commonly used as a first-line in cases of depression with comorbid cardiovascular disease.
Longer-term studies support its ability to reduce relapse rates. At least three randomized controlled trials examined efficacy for relapse prevention over 18 months. Sertraline offered significant beneficial effects.
One study in moderate cases of depression found sertraline was only somewhat superior to Rhodiola rosea over a period of 12 weeks. Rhodiola had fewer negative effects.
Efficacy has been shown in depression associated with traumatic brain injury.
Meta-analyses
Paper 1 – 35 trials from 1980 to 2011
- Similar response rates between sertraline, escitalopram, and paroxetine.
Paper 2 – 10 studies with 2687 MDD patients
- Escitalopram had a greater overall treatment effect vs. sertraline.
Paper 3 – 16 randomized trials with 4569 patients
- Escitalopram was found to be more effective than other SSRIs (citalopram, fluoxetine, paroxetine, sertraline) and SNRIs (venlafaxine, duloxetine).
- The greatest difference was between escitalopram and citalopram. Sertraline was between them.
Paper 4 – Cochrane review of 59 RCTs with 10,000 patients
- Trend in favor of sertraline over other antidepressants in terms of efficacy and tolerability.
PTSD
Some trials have yielded postive results and others have found no notable effect.
One paper found a lack of efficacy in children and adolescents with PTSD.
Studies
Paper 1 – 12-week double-blind placebo-controlled
- 187 outpatients with PTSD
- Mean duration of illness of 12 years
- Randomized to flexible dose sertraline (50 – 200 mg/d) following initial week with 50 mg/d
- Sertraline had significantly greater improvement on 3/4 primary outcome measures.
- 53% response rate vs. 32% with placebo.
- Significant efficacy on CAPS-2 total severity score from Week 2 onward.
- Insomnia was the only negative reported significantly more than with placebo.
Paper 2 – 10-week double-blind placebo-controlled
- 62 military veterans
- Significant improvement on 3/3 efficacy measures: IES-R, CGI-I, CGI-S.
- Significantly greater reduction in the mean score of each of the DSM-4 clusters of the IES-R subscales: reexperiencing/intrusion, avoidance/numbing, and hyperarousal.
Dysthymic disorder
Several randomized trials have shown 12 weeks of flexible-dose sertraline if effective, even in cases of longstanding dysthymia.
It has a similar efficacy to imipramine and may be better tolerated.
Social anxiety disorder
Evidence supports its efficacy for psychic and somatic symptoms.
Studies
Paper 1 – 12-week double-blind, placebo-controlled
- 211 patients with flexible-dose sertraline and 204 with placebo
- Sertraline had a significantly higher response rate and improvement.
- 47% response vs 26%
- Greater decrease in mean LSAS score.
- Among Week 12 completers, the mean change in LSAS was significantly greater, as was the percentage of CGI-I responders.
Paper 2 – 20-week double-blind, placebo-controlled
- 204 adults with SAD
- Initially sertraline 50 mg/d or placebo
- After 4 weeks, the dose could increase by 50 mg/d every 3 weeks if clinically indicated.
- By the end, the mean dose was 146.7 mg.
- Demonstrated superior efficacy relative to placebo.
- 53% response rate vs 29%.
Paper 3 – 24-week double-blind, placebo-controlled
- 387 patients with at least moderate social phobia
- 50 to 150 mg of sertraline or placebo for 24 weeks
- Sertraline patients were significantly more improved than placebo patients.
Anxiety
Evidence supports its status as more effective than placebo.
Study
Paper 1 – 12-week double-blind, placebo-controlled
- 146 sertraline patients completed study, 139 completed it with placebo.
- Flexible-dose for sertraline, with a mean endpoint dose of 95.1 mg/d.
- Sertraline had significantly higher efficacy from Week 4 onward on all primary and secondary outcome measures.
- Significantly higher treatment responder rate, remission rate, and improved quality of life.
- Adverse effects (over 3% and higher than placebo)
- Sweating, nausea, decreased libido in women.
Alcohol addiction
It’s been tested on its own and in combination with naltrexone, with the goal of boosting naltrexone’s effect, especially in those with alcohol addiction and depression.
Evidence for sertraline notably reducing drinking on its own is basically absent, but it might address depression in alcohol-dependent individuals.
If there’s any benefit of SSRI monotherapy, it’s shown up more in less severe drinkers taking 200 mg of sertraline.
Tobacco addiction
It’s been tested, particularly in those with a history of depression.
One study found it reduced the intensity of withdrawal, but it didn’t significantly impact abstinence rates.
OCD
Significant benefit has been seen with 50 to 200 mg/d.
Benefit appears to be maintained in the long-term for many responders.
High doses of 250 to 400 mg/d were shown to be effective in patients unresponsive to initial standard treatment with lower-dose sertraline. The higher doses had a similar apparent safety profile.
Some evidence that CBT is more effective than 100 mg of sertraline.
For adolescents and children
Efficacy has been shown in OCD.
It also appears effective for anxiety in some cases.
Study
Paper 1 – 12-weeks placebo-controlled
- 7 to 17 years old with separation/generalized anxiety or social phobia.
- 440 completed assessment at 12 weeks.
- Rates for “very much improved” or “much improved” on the CGI-I scale at the endpoint:
- Combo of CBT and sertraline: 80.7%
- CBT: 59.7%
- Sertraline: 54.9%
- Placebo: 23.7%
- Indicates it is effective in the short-term for multiple types of childhood anxiety relative to placebo.
- Combo with CBT may be most effective.
- Adverse effects
- No greater suicidal or homicidal ideation over placebo.
- More insomnia, fatigue, sedation, and restlessnesss.
Tolerance
Efficacy declines over long periods of time in general, but it’s maintained to a useful degree in many patients.
It appears there is a notable rise in the risk of relapse over a period of months and years.
Negatives
Most common negatives
At least 1% of patients experience the following: agitation, insomnia, sexual dysfunction, drowsiness, dizziness, headache, increased sweating, dry mouth, and dyspepsia.
It may temporarily lead to anxiety and agitation in a subset of patients during the initial phase of treatment before giving way to anxiolysis. This may fit with a finding that acute SSRI administration seems to increase threat processing in healthy volunteers.
Hypotension has sometimes been seen when treatment first begins and it’s usually transient. Trials often don’t record any instances of hypotension, so it appears quite rare.
There are rare reports of diplopia, blurry vision, mydriasis, anisocoria, abnormal bleeding, and psychotic symptoms like auditory hallucinations and paranoid ideation.
Compared to other treatments
Sexual dysfunction was shown to be less significant with sertraline and fluoxetine relative to paroxetine, citalopram, and venlafaxine in one multicenter study. Though it was markedly higher than with nefazodone or mitrazapine.
Escitalopram and sertraline have overall superior tolerability profiles relative to other common antidepressants. Escitalopram appears to result in less sexual dysfunction than sertraline.
Multiple pieces of research have pointed towards it leading to less weight gain relative to paroxetine. Though the rate of diarrhea is higher.
It may also have less constipation, fatigue, decreased libido in women, and micturition problems vs. paroxetine.
VS TCAs
Significantly lower drowsiness, amnesia, dizziness, constipation, micturition disorders, and general fatigue than amitriptyline.
No apparent differences with insomnia, agitation, headache, dyspepsia, and palpitations.
Possibly higher nausea and insomnia with sertraline vs. amitriptyline.
Sexual dysfunction
Like with other SSRIs, sexual dysfunction can occur, possibly due to 5-HT2 and 5-HT1 receptor agonism.
It tends to persists over time, unlike other negatives.
These problems are highly associated with treatment nonadherence.
Among the problems are anorgasmia, decreased libido, delayed ejaculation, and decreased pleasure.
A double-blind controlled study found orgasm difficulties in 47% of females and 67% of males.
A double-blind controlled study found decreased libido in 21% of females and 22% of males.
Mania and hypomania
There have been some relatively rare reports of mania and hypomania, including in children and adolescents. In some cases just 25-50 mg/d was enough to trigger the response.
Neurogenesis & neuroprotection
A role of neurogenesis and synaptogenesis may exist in the beneficial effects of SSRIs like sertraline.
Studies have indicated neurogenesis is associated with beneficial effects in mice.
It appears SSRIs can affect signalling pathways that regulate neuroplasticity and cell survival.
There may be a protective effect against neurodegeneration caused by oxidative stress and disrupted energy metabolism.
An upregulation of BDNF is seen with sertraline treatment.
Studies
Paper 1 – Sertraline promoting rat hippocampus-derived neural stem cells differentiating into neurons & attenuating some cellular damage.
- It promoted NCS differentiation into serotonergic neuronal cells at 5 uM.
- It inhibited NCS differentiation into glial cells.
- Protected against LPS-induced cellular damage (LPS is proinflammatory) at 5 uM.
Paper 2 – Slowed disease progression and increased neurogenesis in an in vivo mouse model of Huntington’s diease
- Rise in BDNF levels, preservation of chaperone protein HSP70 levels, preservation of anti-apoptotic Bcl-2 levels, restoration of depleted serotonin, retarded motor behavioral impairment, enhanced neurogenesis, and increased survival.
- Appears the rise in neurogenesis mediated the beneficial effects.
- Blocking neurogenesis removed the beneficial impact on motor function and reduced survival extension.
- Effective dose level was similar to what’s considered safe and achievable in humans.
Paper 3 – Attenuation of postischemic brain injury in mice
- Dose of 20 mg/kg (IP) began 1 hour after ischemia and continued for 14 days.
- Significantly reduced damage following photothrombotic cortical ischemia.
- Restored CBF autoregulation.
- Elevated expression of HIF-1a and HO-1 proteins.
- Relevance
- Could be useful post-stroke to reduce depression and improve recovery.
Chemistry & Pharmacology
Chemistry
Sertraline is an isomer of a tametraline derivative.
Pharmacology
It has a primary effect of inhibiting reuptake of serotonin. Some dopamine reuptake inhibition also exists, though it’s of unclear clinical relevance.
The therapeutic activity of sertraline comes from processes more complex than simply inhibiting serotonin uptake. Most of the hypotheses have to do with neuroadaptations resulting from prolonged exposure to the drug.
Some of the possibilities are 5-HT1A autoreceptor desensitization (boosting serotonin activity), decreasing serotonergic and glutamatergic activity, and causing neurogenesis and synaptogenesis.
There’s an immediate effect on serotonin, yet the medical benefits take longer to appear. It’s believed the adaptations are responsible for that delay.
To achieve a 250% increase in extracellular serotonin, SERT occupancy must be 70% for escitalopram, 83% for paroxetine, and 95% for sertraline.
Hypotheses
BDNF/neurogenesis
A lot of attention has been given to the impact of SSRIs on BDNF, a protein associated with the support of neurons and the growth/differentiation of new neurons and synapses.
BDNF increases can be seen with sertraline and other antidepressants. Lower basal levels of BDNF are also seen in depression.
One study found sertraline significantly increased serum BDNF levels after 5 weeks and that was sustained after 6 months, nearly normalizing the patients.
With neurogenesis enhanced, shrinkage seen in depression could be reversed.
Problems do exist with this hypothesis. Namely, some antidepressants don’t really affect BDNF, yet they’re still effective.
High serotonin
Some evidence exists in support of the idea that depression is a serotonin-influenced state, whose high activity diverts resources towards cognitive processes like rumination and away from activities like growth and reproduction.
Melancholia is highly associated with sustained HPA axis activation, suggesting it’s an energetically expensive state.
An initial rise in serotonin from SSRIs may aggravate symptoms, while prolonged treatment leads to useful adaptations.
Acute SSRI treatment raises serotonin transmission to the prefrontal cortex (PFC), causing an increase in glutamatergic activity. This has been shown in rodents.
Longer-term treatment can eventually drop extracellular serotonin levels. Chronic treatment could then reduce glutamatergic activity.
In rats, the symptom-reducing effects of chronic desipramine (a TCA) administration were associated with reduced total (intracellular and extracellular) serotonin content in the PFC, hippocampus, and nucleus accumbens.
In primates, a microdialysis study found extracellular serotonin levels in the hippocampus and other regions returned to baseline with chronic fluoxetine administration.
Given these lines of evidence, the hypothesis is that chronic administration serves to reverse elevated glutamatergic activity that’s initially boosted by SSRIs.
Information processing
SSRIs seem to impact low-level information processing, moving it towards positive vs. negative associations.
This can be taken as a “bottom-up” impact on emotional processing.
Relearning as a result of these changes could take weeks, possibly contributing to the therapeutic lag time.
Relearning could be connected to effects on synaptic plasticity.
Dopamine activity
Sertraline was found to significantly increase spontaneous locomotor behavior in animals at doses that produce 5-HT reuptake inhibition. Paroxetine and escitalopram were devoid of this effect.
The drug increased extracellular dopamine in the nucleus accumbens and striatum of rats at clinically relevant doses. This wasn’t seen with other SSRIs.
It also boosted extracellular norepinephrine levels in the nucleus accumbens, possibly from dopaminergic activity.
Pharmacokinetics
Half-life: 24 to 27 hours
Desmethylsertraline half-life: 66 hours
Extensive metabolism in the liver. The primary metabolite is desmethylsertraline, which is 5-10x less potent with its activity.
CYP2B6 is the primary enzyme involved, though it’s not the only one.
History
1977
Kenneth Koe, a chemist in the Pfizer pharmacology department, was looking at structural features of potent and relatively selective uptake inhibitors.
He worked with Willard Welch to examine a set of of tametraline derivatives.
Those derivatives were tested and sertraline was picked from the group due to its selective and potent nature.
1979
Patented by Pfizer.
1980s
In vitro and in vivo research was carried out, showing sertraline was an effective serotonin uptake blocker and could be absorbed orally.
The studies confirmed it was largely devoid of non-serotonin actions and didn’t inhibit MAO.
Up to 400 mg/d could be tolerated in humans and the substance led to fewer side effects than TCA antidepressants.
1990s
Sertraline was approved in the UK in 1990.
The FDA approved it for clinical use in 1991. Sertraline entered the market in February 1992 under the name Zoloft.
1990s – 2000s
It was investigated and adopted for many uses around the world.
During the early part of its history, sertraline was one of the only SSRIs on the market, alongside fluoxetine, paroxetine, and fluvoxamine.
Many health professionals were unaware of some of its problematic aspects, particularly its withdrawal symptoms. This was connected with a lack of knowledge among patients as well.
~2005
The drug was generating revenue of $2 to $3 billion per year.
2013
Sertraline was the most popular antidepressant in the US with over 40 million prescriptions. It was the second most popular psychiatric medication.
Legal Status
US (as of February 2017)
Unscheduled. Prescription-only.
Other countries (check your local laws)
Generally unscheduled or prescription-only.
Safety
Negatives
Most of the negatives in medical settings are fairly mild.
It may increase panic and anxiety, though this can be followed by a therapeutic anxiolytic action.
Some of the negatives include nausea, insomnia, sexual dysfunction, dyspepsia, sweating, and diarrhea.
Rare problems
There are rare cases of abnormal bleeding, pancreatitis, hepatitis, significant tremor, galactorrhea, syncope, and sinus arrest.
Not all of those have been definitively connected to sertraline, but they’ve been associated with its use in a small portion of users.
Overdose
The drug is largely safe in fairly large overdose.
Some of the symptoms include drowsiness, tachycardia, tremor, nausea, vomiting, and mydriasis.
Compared to TCAs, antidepressant-only death from overdose is much less common with SSRIs. The majority of cases involve additional drugs.
Reviews
1 – Analysis of 52 cases of sertraline-only overdose
- Mean dose of 727 mg
- No significant symptoms in 34 cases.
- Symptomatic patients had mild CNS, cardiovascular, and gastrointestinal effects.
2 – Analysis of 40 overdoses
- Mean dose of 1,579 mg.
- Median of 1,400 mg.
- Range of 50 to 8000 mg.
- 17 sertraline-only ingestions, 10 of which were asymptomatic.
- Tremor was the primary symptom in the others.
3 – Manufacturer reported ingestions up to 2,600 mg in four patients with suicidal intent
- All required minimal treatment.
Suicide
There’s conflicting evidence about the impact of SSRIs and sertraline specifically on suicidal thoughts and action.
Most data suggests it’s a very low risk for all patients. SSRIs may slightly increase the risk in people under the age of 24 and have a neutral or positive impact over the age of 24.
Even though it’s rare, there are cases of sudden onset aggression and suicidal ideation. Prescribers should be particularly focused on monitoring patients for the first 1-2 months of treatment.
Sertraline appears to have an even lower risk than some antidepressants, such as venlafaxine.
Interactions
CYP2D6 inhibition
Inhibition of CYP2D6 was found to result in 2 to 10-fold higher level of a TCA.
This could have an impact on other drugs reliant on CYP2D6 for metabolism.
Antiplatelet drugs
SSRIs are known to be a risk factor for hemorrhage and that risk could further increase when combined with antiplatelet drugs like acetylsalicylic acid (ASA) or clopidogrel.
This comes from SSRIs inhibiting serotonin uptake into platelets, thereby significantly reducing serotonin concentrations in platelets. Serotonin plays an important role in the aggregation of platelets.
The risk of problematic responses is still low, but it should be considered.
Liver disease
Chronic liver disease and cirrhosis have been shown to affect the pharmacokinetics of sertraline.
Studies
Paper 1
- 10 patients with chronic hepatic insufficiency from cirrhosis.
- Cmax increased 1.7-fold
- Cmax of desmethylsertraline decreased 1.5-fold
- No significant difference in the Tmax of sertraline.
- Tmax of desmethylsertraline was significantly longer.
- The elimination half-life was 2.5x longer.
Cardiovascular
Although it’s less problematic than TCAs, some cardiovascular issues may still arise, mainly in overdose. The primary effect is tachycardia and ECG changes have sometimes been recorded.
Studies
Paper 1 – Impact on cardiac ion channels in vitro
- It inhibited ion channels
- IC50s
- hERG – 0.7 uM
- IK1 – 10.5 uM
- IKs – 15.2 uM
- IC50s
- The hERG IC50 is close to the mean peak plasma concentration in once-daily dosing of 200 mg, which is about 0.6 uM.
Hepatic
A premarketing study showed 0.8% of participants had elevations in serum transaminase by the first week, gradually returning to normal upon drug withdrawal.
Typically the drug has no effect on liver function or such a minimal effect that discontinuation isn’t warranted.
There have been a few cases of liver toxicity, though it’s difficult to figure out sertraline’s importance in some.
It’s a very rare response regardless of dose. Over 100 mg might be somewhat riskier than under 100 mg.
The mechanism has been hypothesized to be immunologic.
Studies
Paper 1 – Disruption of liver mitochondria in rat primary hepatocytes in vitro
- ATP depletion was observed within 0.5 hours, a sign of mitochondrial dysfunction.
- Prolonged or worsening ATP depletion can lead to irreversible mitochondrial damage and necrotic cell death.
- Mitochondrial swelling could be prevented with an ANT inhibitor, but not a CypD inhibitor.
- Indicating adenine nucleotide translocase (ANT) could be the primary target for the mitochondrial permeability transition pore (MPT) induction that was observed, with the mitochondrial swelling as the indicator.
- MPT induction via ANT appears to be the likely mechanism for sertraline hepatotoxicity.
- However, the concentration is higher than what’s seen clinically.
- A single 400 mg dose in healthy people leads to a 0.253 ug/mL plasma concentration (0.74 uM)
- But the study was using 37.5 uM
- Studies looking for relevant hepatotoxicity do use concentrations above what’s seen clinically. So, the finding was still considered meaningful.
Non-fatal cases
Case 1
- 23-year-old female
- Presented for evaluation of hepatitis
- Had been taking sertraline for depression and acetaminophen for headaches/pain.
- At presentation
- Temperature of 37.89°C (100.2°F) and mildly orthostatic
- Blood test showed elevated serum ALT
- Therapy with sertraline ended and her symptoms resolved.
- Three days later
- Returned with recurrent nausea and vomiting
- Serum ALT level remained elevated
- Presumed that liver disease was to blame.
- Liver biopsy demonstrated changes consistent with drug-induced or autoimmune-induced hepatitis.
- Diagnosed with autoimmune hepatitis, given 20 mg prednisone oral per day.
- Four weeks post-sertraline cessation
- Serum ALT near normal
- Resumed sertraline for depression two weeks later
- Followed by increasing fatigue.
- Three weeks after resuming sertraline
- Serum ALT had risen again significantly
- Both sertraline and prednisone stopped
- ALT levels returned to normal within 89 days
- Depression treated with amitriptyline after that point without issue.
Case 2
- 17-year-old male
- Using sertraline 25 mg/d for depression for 6 months
- Presented with nausea, fatigue, scleral jaundice, and dark urine.
- Significant increase in aminotransferase (AST/ALT)
- Sertraline discontinued and levels returned to normal range within 6 months.
Fatal cases
Case 1
- 54-year-old male
- Admitted on November 3 for acute alcohol withdrawal syndrome–he had been abusing alcohol for over 10 years.
- Given diazepam
- November 20
- Referred to department of psychiatry for depression
- Given sertraline 50 mg BID (100 mg/d), which was in addition to ongoing diazepam.
- Liver enzymes at this time were normal except for elevated serum yGT.
- Two weeks later
- Complained of fatigue, developed jaundice and somnolence.
- December 8
- Admitted to ICU
- Diazepam and sertraline were discontinued.
- Over the next week
- Liver status worsened
- Died on December 17
- Postmortem showed extensive hepatocyte necrosis with formation of bridges linking portal tracts together and to terminal hepatic venules.
- Sertraline was considered the trigger for the acute liver injury.
- Mechanism unknown
Serotonin syndrome
It could potentially occur with sertraline by itself, generally with a very large overdose (though there are outlier reports). It’s mainly a concern when other serotonergic drugs are used.
Rare reports of it occurring with low therapeutic doses, such as a 9-year-old given a single 50 mg dose.
MAOIs and l-tryptophan are among the things that should be avoided.
Normally it resolves within 24 hours, but there are reports of delirium and other effects persisting for days.
Even relatively weak MAOIs like linezolid have been problematic.
Cases
Case 1
- 47-year-old female
- On sertraline 100 mg/d for over a year
- Linezolid 600 mg every 12 hours added
- Clinical pharmacist explained the potential interaction to prescriber, but combo went forward anyways.
- Fourth day of linezolid
- Incoordination, confusion, and hypertension.
- Symptoms went away within 4 days of removing linezolid.
- Another round of treatment with linezolid, but with sertraline removed on Day 1.
- Nine days into treatment: delirium, confusion, incoordination, myoclonus, then cardiopulmonary arrest, and patient in coma with anoxic brain injury.
- Linezolid discontinued
- Cyproheptadine, a serotonin antagonist, was started.
- Relieved symptoms within a few days.
Withdrawal
Withdrawal is common in medical settings. It’s typically mild and short-lived.
The syndrome isn’t specific to SSRIs, having also been reported with MAOIs, TCAs, and SNRIs over the decades.
Usually it appears within a few days of stopping or reducing your dose. It then resolves between 1 day and 3 weeks after the onset, with a common duration of about 5-8 days.
If withdrawal is significant, restarting the medication can usually eliminate the symptoms within 24 hours.
Withdrawal doesn’t occur for everyone and the actual prevalence is unknown. It’s also unknown why most people experience mild short-lasting symptoms while a minority have prolonged or severe symptoms.
Symptoms
The primary ones are: flu-like symptoms, anxiety, emotional lability, insomnia, decreased concentration, irritability, headache, dizziness, light-headedness, and nausea.
Electric shock sensations are fairly common and of variable intensity and duration.
Severe and rare symptoms include: mania, hypomania, extrapyramidal symptoms, ataxia leading to falls, fatigue causing difficulty walking, electric shock sensations that impair walking and driving.
Rebound
It’s possible to experience rebound depression or anxiety, meaning the original problems return with greater intensity following cessation. Typically this effect is only present for a short time.
Prolonged
Longer-lasting issues persisting for more than 6 weeks are rare, but they’ve sometimes been reported. These include disturbed mood, depression, emotional lability, mood swings, irritability, insomnia, anxiety, impaired concentration, and impaired memory.
The issues may be distinct from the patient’s original condition.
This might be somewhat less common with sertraline compared to other SSRIs.
Tapering
Tapering is a useful strategy to potentially reduce the severity of symptoms.
People often still report symptoms to some extent once they actually end their use, even after a long taper.
Risky combinations (list may not be complete)
Dextromethorphan, Tramadol, and MAOIs.
Overdose cases
Case 1
- 51-year-old female
- History of depression and alcohol abuse
- 3 days prior to admission
- Entered ED for acute alcohol intoxication
- Admitted to hospital after being found in somnolent state near several open bill bottles.
- She could have taken up to 8 grams of sertraline.
- Presented with:
- BP: 132/83
- HR: 101
- Respiratory rate: 18
- Temperature: 36.9 C (98.5 F)
- Dilated pupils, brisk reflexes, and unsustaind ankle clonus bilaterally.
- Somnolent but arousable
- Denied memory of the overdose
- Serum creatine kinase (CK) was elevated
- Levels upon admission
- Serum in serum: 2.93 ug/mL
- Desmethylsertraline in serum: 1.68 ug/mL
- Other drugs at admission
- Norpropoxyphene in serum: .268 ug/mL
- Within therapeutic range
- Nortriptyline in serum: .026 ug/mL
- Below therapeutic range
- Norpropoxyphene in serum: .268 ug/mL
- Hospital Day 3
- Patient had an acute mental status change with agitation, disorientation, and visual hallucinations suggested by her grasping at the air.
- BP: 150/115
- HR: 88
- Temperature: 38.5 C (101.4 F)
- Hyperreflexia and sustained ankle clonus bilaterally but no muscle rigidity.
- Hospital Day 4
- Received 2 doses of benzodiazepines, diazepam and oxazepam.
- Partly relieved agitation.
- Sertraline in serum: .453 ug/mL
- Desmethylsertraline in serum: 1.132 ug/mL
- Received 2 doses of benzodiazepines, diazepam and oxazepam.
- Hospital Day 5
- Sertraline in serum: .305 ug/mL
- CK and liver enzyme levels returned to normal
- Hospital Day 6
- Received 1 oral dose of zolmitriptan at 2.5 mg
- Discharged after receiving psychotherapy.
- Not believed any other drugs played a role.
- Primary diagnosis of serotonin syndrome resulting from very large sertraline overdose.
Case 2
- 5-year-old female with no medical history
- Brought to ED after ingesting at least 400 mg of sertraline
- Vomited once pre-evaluation
- She said she was “jittery”
- Also muscle twitching and felt her “heart was beating fast.”
- Evaluation
- Alert, 39.1°C (102.4°F) temperature, diaphoretic, tachycardic at 177, hypertensive 158/90, and tachypneic 24 b/m
- Dilated pupils
- Received gastric lavage and charcoal.
- Psychiatric consultation the following day due to her saying she was worried about dying from her “heart beating so fast.”
- Day 2
- Drowsy, but arousable.
- Because the symptoms were resolving, she was discharged from the hospital about 48 hours post-administration.
- Although her mother felt she was still “not herself.”
- Day after discharge
- Readmitted
- Irritability, agitation, tachycardia, poor sleep, poor attention, and unusually combative.
- Sertraline level was 0.099 ug/mL (about 72 hours post-administration)
- During the week
- Intermittent fever, mild tachycardia, mild hypertension, mood swings, hyperactivity, and generally impulsive/disinhibited behavior.
- Symptoms resolved gradually over a 7-day period and she was discharged again.
- Mother said symptoms went away entirely within a month.
Case 3
- 9-year-old male
- History of ADHD and treatment with methylphenidate, which had stopped 9 days prior.
- Lived with mother who was prescribed sertraline.
- Pre-admission
- Reported “chills” and two episodes of vomiting.
- In ED
- BP of 100/66, Temp of 38.5°C (101.3°F), HR of 176 and irregular, tachypnea of 38 b/m
- Alert, uncooperative, rambling, and having hallucinations.
- Very agitated–was biting his hands and arms and trying to bite the examiner.
- Eventually transferred to pediatric ICU due to persistent symptoms
- HR over 200 and temperature of 42.4°F (108°F)
- Hallucinations continued alongside motor agitation.
- Clammy skin and shaking in extremities and writhing.
- High CK value
- Received
- 3 mg lorazepam, 650 mg acetaminophen, and 975 mg chloral hydrate.
- Writhing gradually subsided, but the shaking activity in the extremities became more intense.
- Pupils were fixed and dilated.
- Due to it being consistent with anticholinergic response
- Given physostigmine 0.5 mg every 10 minutes, totaling 2 mg
- Appropriate response of reduced heart rate and temperature.
- Day 2
- Excessive tonic movements of the extremities and face.
- Rigidity in the upper and lower extremities.
- Temperature near normal post-acetaminophen and cooling blankets.
- Mental status improved, but still hallucinations.
- High CK level remained
- Day 3
- Generally alert with normal muscle activity and vital signs.
- Day 4
- Alert and fully oriented.
- Stable vital signs with only a mild tremor still present.
- Concentrations of sertraline in serum
- Day 1 (9 hours post-administration): 0.068 ug/mL
- Day 2 (26.5 hours): 0.032 ug/mL
- Day 3 (50.5 hours): Under 0.010 ug/mL
- Day 4 (74.5 hours): Under 0.010 ug/mL
References
(2015) The pharmacokinetics of sertraline in overdose and the effect of activated charcoal.
(2015) Serotonin syndrome precipitated by sertraline and discontinuation of clozapine
(2015) Seeing double: sertraline and diplopia: a case report.
(2015) New Classification of Selective Serotonin Reuptake Inhibitor Withdrawal
(2014) A comparative review of escitalopram, paroxetine, and sertraline: Are they all alike?
(2013) Serotonin syndrome after sertraline overdose in a child: a case report.
(2013) Sertraline and mirtazapine as geriatric antidepressants.
(2013) Sertraline-induced ventricular tachycardia.
(2013) Sertraline-induced galactorrhea: case report and review of cases reported with other SSRIs.
(2012) Mitochondrial dysfunction induced by sertraline, an antidepressant agent.
(2012) Wide spectrum of inhibitory effects of sertraline on cardiac ion channels.
(2011) Antidepressants, antiplatelets and bleeding: One more thing to worry about?
(2010) Sinus arrest due to sertraline.
(2010) Sertraline-related anisocoria.
(2010) The use of antidepressants in pregnant and breastfeeding women: a review of recent studies.
(2010) A possible explanation for dizziness following SSRI discontinuation.
(2010) Sertraline hepatotoxicity: report of a case and review of the literature. [Comment]
(2009) An evidence-based review of the clinical use of sertraline in mood and anxiety disorders.
(2009) A double-blind, placebo-controlled study of sertraline with naltrexone for alcohol dependence.
(2009) Sertraline versus other antidepressive agents for depression.
(2009) Fluoxetine and sertraline attenuate postischemic brain injury in mice.
(2009) Sertraline hepatotoxicity: report of a case and review of the literature.
(2008) Cognitive Behavioral Therapy, Sertraline, or a Combination in Childhood Anxiety
(2008) Serotonin syndrome following a single 50 mg dose of sertraline in a child.
(2007) Inappropriate sexual behaviour in a case of ALS and FTD: successful treatment with sertraline.
(2007) Recognising and managing antidepressant discontinuation symptoms
(2007) Suicidal thinking and behavior during treatment with sertraline in late-life depression.
(2006) Clinical review: Relationship between antidepressant drugs and suicidality in adults
(2006) How Can We Know Whether Antidepressants Increase Suicide Risk?
(2006) Sertraline and gastrointestinal bleeding in an adolescent girl.
(2006) The nature of the discontinuation syndrome associated with antidepressant drugs.
(2006) Sertraline treatment of co-occurring alcohol dependence and major depression.
(2006) Genital anaesthesia persisting six years after sertraline discontinuation.
(2005) A placebo-controlled, randomized withdrawal study of sertraline for panic disorder in Japan.
(2005) QT interval prolongation after sertraline overdose: a case report.
(2005) The brains behind blockbusters.
(2005) Sertraline in the treatment of co-occurring alcohol dependence and posttraumatic stress disorder.
(2004) Efficacy of sertraline in a 12-week trial for generalized anxiety disorder.
(2004) Treatment of bulimia nervosa with sertraline: a randomized controlled trial.
(2004) Sertraline as a treatment for PTSD: a systematic review and meta-analysis
(2003) Sertraline-induced hypomania: a genuine side-effect.
(2003) Sertraline for social anxiety disorder.
(2002) Up-regulation of tryptophan hydroxylase expression and serotonin synthesis by sertraline.
(2002) A randomized trial of sertraline as a cessation aid for smokers with a history of major depression.
(2002) Sertraline treatment of major depression in patients with acute MI or unstable angina.
(2001) Acute fatal hepatitis related to sertraline
(2001) Parkinsonism and Parkinson’s disease associated with long-term administration of sertraline.
(2001) Comment: sudden cardiac death with clozapine and sertraline combination.
(2001) Sudden cardiac death with clozapine and sertraline combination.
(2000) Massive sertraline overdose.
(2000) Sertraline in the treatment of major depression following mild traumatic brain injury.
(1999) Serotonin syndrome in a child associated with erythromycin and sertraline.
(1998) Fatal Multiple Drug Intoxication Following Acute Sertraline Use
(1998) Interaction of sertraline and moclobemide induces the serotonin syndrome in the rat
(1998) Sertraline in the treatment of premature ejaculation: a double-blind placebo controlled study.
(1997) Pharmacology of the Selective Serotonin Reuptake Inhibitors in Children and Adolescents
(1997) Serotonin syndrome after sertraline overdose in a 5-year-old girl.
(1997) Sertraline and psychotic symptoms: a case series.
(1996) Analysis of sertraline-only overdoses.
(1996) Sertraline withdrawal in two brothers: a case report.
(1996) Sertraline overdose.
(1996) Orthostatic hypotension induced by sertraline withdrawal.
(1996) Influence of liver cirrhosis on sertraline pharmacokinetics.
(1995) Discovery and preclinical development of the serotonin reuptake inhibitor sertraline
(1995) Suspected congenital sertraline dependence.
(1994) Sertraline intoxication in a child.
(1994) Sudden chest pain with sertraline.
(1991) Clinical implications of the pharmacology of sertraline.
(1986) Double-blind dose determination study of a new antidepressant—sertraline